Int J Obstet Anesth:剖腹产Tarlov囊肿如何进行脊髓麻醉?
2019-01-25 汐雨 医博士
Tarlov囊肿高发,向麻醉科医师提出了挑战。周围神经囊肿可导致脊髓麻醉失败。Tarlov囊肿的相关症状可以被分娩期镇痛麻醉所掩饰或诱发。近期,International Journal of Obstetric Anesthesia杂志上报道了一例24岁行剖宫产的Tarlov囊肿患者,成功地进行了麻醉。
周围神经(Tarlov)囊肿是脑膜的病理性扩张,形成于周围神经和神经内膜之间。Tarlov囊肿发生在背根神经节的脊神经上(图1)。Tarlov囊肿可发生于10%的成年人中,随着改进的磁共振成像和计算机断层扫描(CT)技术的出现,该病可以确诊。
图1:神经周围囊肿的示意图
Tarlov囊肿高发,向麻醉科医师提出了挑战。周围神经囊肿可导致脊髓麻醉失败。Tarlov囊肿的相关症状可以被分娩期镇痛麻醉所掩饰或诱发。近期,International Journal of Obstetric Anesthesia杂志上报道了一例24岁行剖宫产的Tarlov囊肿患者,成功地进行了麻醉。
病例介绍
孕妇24岁(G2P0,以前有流产史),体重80kg,身高174cm。在孕40周时来我院行剖腹产手术。S1水平左侧Tarlov囊肿(18?mm?×?16?mm?×?12?mm)。囊肿的发展无明确因素(如结蹄组织疾病或外伤),患者称自己大概每3个月就有1次头疼、背痛和压迫性坐骨神经痛,采用扑热息痛、可待因进行镇痛,行囊肿引流术,注射类固醇与局部麻醉剂混合使用。
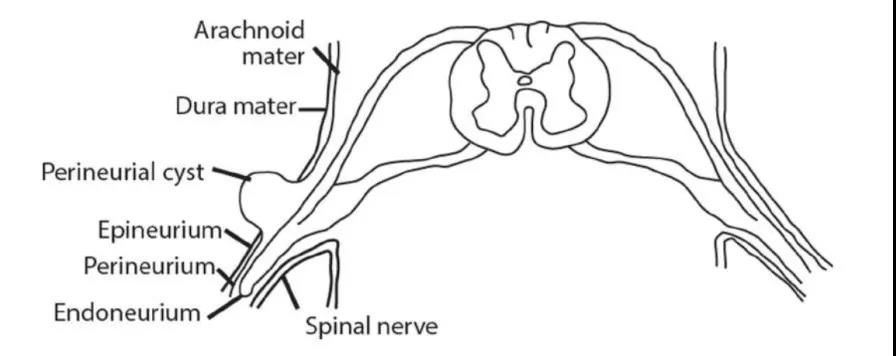
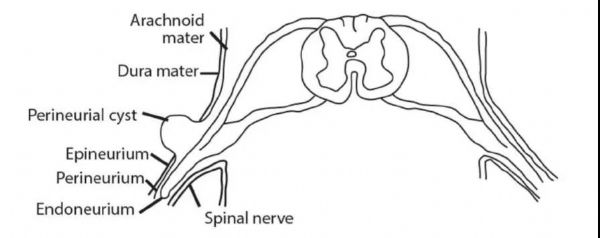
患者分娩前18个月,接受CT引导下注射类固醇(地塞米松8毫克,2毫升),布比卡因(0.5毫升0.5%)在L5-S1水平。2个月后CT引导下引流,引流出2mL脑脊液,用5毫升血液进行硬膜外血液补片,以减少硬脑膜穿刺后头痛的风险(图2,图3)。在分娩前十三个月,在CT透视下排出2毫升液体,并进行重复的血液补片。
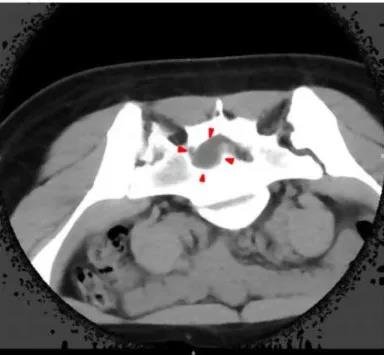
图2:剖宫产术前18个月,患者S1神经根显示左侧神经管囊肿

图3:CT透视图像,剖宫产术前18个月,患者左侧S1神经管囊肿
鉴于患者未侵犯腰椎且没有神经症状,考虑剖腹产时采用标准的单次脊髓麻醉。在麻醉时,应用无菌技术,包括长袍、无菌手套、窗帘和用氯己定2%与酒精制成的皮肤制剂。采用5ml 1%利多卡因进行局部浸润,27G针顺利插入L3-4间隙。0.5%布比卡因、20μg芬太尼、100μg鞘内注射吗啡后,剖宫产手术顺利,无需进一步干预或抢救镇痛。
术后未见严重并发症,电话随访6个月后,患者偶尔有乏力、头疼等症状。此外,她经历的间歇性双侧腰痛,与坐姿有关。这些症状被认为与继发性肾积液囊肿积液有关。
鉴于Tarlov手术有风险和术后康复耗时,神经外科医师建议继续进行囊肿引流。
讨论及小结
当Tarlov囊肿位于骶骨时,脊髓麻醉是一种可行的产科选择,如果囊肿位于腰部时,麻醉风险和神经损伤的发生率就比较高,这种情况下,全麻可能作为首选。
产科麻醉师必须对患者进行评估,包括囊肿的大小、位置、神经病变的严重程度,综合地进行判断,以选择合适的麻醉方式。
原始出处:
Pfund N, Oh A, Cyna A, et al. Successful spinal anaesthesia in a patient with a Tarlov cyst. International Journal of Obstetric Anesthesia. 2018; 34:96-98. doi:10.1016/j.ijoa.2017.10.004.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#EST#
31
#脊髓麻醉#
32
#TET#
37
#囊肿#
29