Molecular Cell:我国研究者干细胞癌变机理获进展
2012-10-09 Molecular Cell Molecular Cell
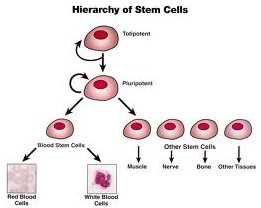
人体中的癌细胞是从哪里来的?这个问题,全世界每天都有数万的科学家在苦苦探寻答案。随着研究的深入,“肿瘤干细胞”这个词也渐渐进入视野中心,但是肿瘤干细胞是如何演变成的,却依然是个谜。最近,浙江大学王英杰、沈炳辉教授的联合课题组在干细胞研究中发现,当两种关键蛋白质“失控”发生越位碰撞后,就会引发一系列变化,将一个正常的干细胞变成肿瘤干细胞。这项揭示干细胞癌变重要机制的研究成果,10月4日在国际生命
人体中的癌细胞是从哪里来的?这个问题,全世界每天都有数万的科学家在苦苦探寻答案。随着研究的深入,“肿瘤干细胞”这个词也渐渐进入视野中心,但是肿瘤干细胞是如何演变成的,却依然是个谜。最近,浙江大学王英杰、沈炳辉教授的联合课题组在干细胞研究中发现,当两种关键蛋白质“失控”发生越位碰撞后,就会引发一系列变化,将一个正常的干细胞变成肿瘤干细胞。这项揭示干细胞癌变重要机制的研究成果,10月4日在国际生命科学领域顶尖杂志《细胞》的子刊《分子细胞》上在线公布。
近年来,科学家们发现,在许多肿瘤组织中存在少数细胞小群体,它们有着与干细胞十分相似的特性,能自我更新,也能分化;同时,它们还有一项特殊的本领,就是“逃逸”。王英杰说:“我们把这种细胞称为肿瘤干细胞。正常的干细胞,在遇到损伤刺激或不良条件时,会很快分化或‘自杀’,而肿瘤细胞中的这些干细胞不但不会‘自杀’,反而会先‘躲’起来,然后再变本加厉地进行‘繁殖’。”这种现象,在一些接受放疗和化疗的肿瘤患者身上表现得十分明显。在药物作用下,肿瘤干细胞表面上似乎是消失了,但一段时间后却又卷土重来,目前的放疗、化疗无法从根本上消灭它们。
“目前的一些证据显示,肿瘤干细胞可能主要来源于正常干细胞的癌变。我们要研究的,就是找出引起干细胞癌变的‘元凶’。”王英杰介绍说,这与转录因子Oct4和蛋白激酶Akt之间可能有直接的联系。Oct4就像一个开关,调控着干细胞中几百个重要蛋白质的合成;而Akt作为一个蛋白激酶,是维持肿瘤细胞生存和增殖最重要的蛋白之一。王英杰与沈炳辉的研究团队经过近3年的努力探索,终于解开了Oct4和Akt在胚胎癌细胞中的互作之谜。
“这两个蛋白质,在正常干细胞中只有微弱或瞬间的碰撞。”王英杰说,“但是在胚胎癌细胞中两者的相互作用就明显增强,Akt能将Oct4‘变异’,变成自己的帮凶,更容易地定位在细胞核内,并促进它与另一干细胞转录因子Sox2形成复合物,增强胚胎癌细胞的自我更新能力。”
“这还只是故事的前半部分”,王英杰说,“更有意思的是,我们发现,在胚胎癌细胞中,Oct4和Akt间彼此结盟,形成了一个相互促进的调控机制,即‘Oct4–Akt正反馈回路系统’。”王英杰认为,这也许是肿瘤干细胞比正常干细胞具有更强的自我更新能力和抗凋亡能力的一个重要原因。
“我们找到了干细胞癌变的一种重要机制,接下来,我们要研究这种机制在肿瘤干细胞中是否存在普遍性。”王英杰指出,如果该机制普遍存在,那么阻断“Oct4–Akt正反馈回路系统”的治疗手段将会为根除肿瘤干细胞和根治癌症带来重大突破。
这些发现揭示了干细胞癌变的一种重要机制,为进一步深入了解肿瘤干细胞发生机理提供了全新的线索。
链接:Yuanji Lin, Ying Yang, Weihua Li, Qi Chen, Jie Li, Xiao Pan, Lina Zhou, Changwei Liu, Chunsong Chen, Jianqin He, Hongcui Cao, Hangping Yao, Li Zheng, Xiaowei Xu, Zongping Xia, Jiangtao Ren, Lei Xiao, Lanjuan Li, Binghui Shen, Honglin Zhou, Ying-Jie Wang.Reciprocal Regulation of Akt and Oct4 Promotes the Self-Renewal and Survival of Embryonal Carcinoma Cells.Molecular Cell, 04 October 2012
拓展阅读:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#癌变机理#
39
#Cell#
28
#CEL#
0
#研究者#
27
#细胞癌#
43
#癌变#
31