Cancers:早期乳腺癌患者新辅助放化疗的长期疗效和安全性
2021-10-18 yd2015 MedSci原创
研究表明,早期乳腺癌新辅助放化疗可取得较高的长期局部控制率以及有限的不良反应。
局限性乳腺癌的标准治疗方法是乳房肿瘤切除术后进行放射治疗,或者当肿瘤较大而无法进行保乳治疗时进行全乳房切除术。这种策略降低了局部复发的风险,提高了患者的总生存率。就生活质量而言,避免全乳房切除术是患者的一个基本目标。在不适合一线保乳手术的患者中,新辅助化疗已被证明在降低分期方面是有效的,但在激素受体阳性的患者中作用较小。此外,新辅助化疗与辅助化疗在总生存期和无病生存期方面均无明显差异。有研究表明新辅助放疗可以达到良好的完全病理缓解率(641%),且安全性良好。S14研究表明新辅助放化疗(5-FU+长春瑞滨)取得病理完全缓解率为27%,且急性毒性耐受。然而,乳房放射治疗已经取得了相当大的进展,包括强度调制放射治疗(IMRT)等。术前放射治疗在某些情况下效果较好,包括(i)降低分期以进行保留手术,(ii)促进乳房重建,(iii)促进部分乳房照射,和/或(iv)协助转化研究。近期,Cancers杂志报道了II期S14研究13年的长期生存和毒性结果。

从2001年到2003年,59名不能接受早期保乳治疗(BCS)的T2-3N0-2M0浸润性乳腺癌(BC)患者被纳入这项前瞻性、非随机II期研究。化疗(CT)包括连续4个周期的5-FU输注和长春瑞滨。与第二个CT周期同时开始,常规分割的放疗RT用于乳腺和淋巴结照射,然后进行乳房手术。
研究人群包括平均年龄49岁的女性[31-65],其中41%为绝经后女性。治疗前MRI报告的病变平均直径为38 mm (20-80 mm), 73%的患者为cT2期,27%的患者为cT3期。组织学主要包括导管癌(68%)和小叶癌(22%),其次是一些较少见的组织学亚型(10%),31%的SBR级别为3, 49%的SBR级别为2。
治疗5年后,没有4级或5级毒性报告,只有1例3级不良反应报告。51例(86%)中位随访13年的患者中,有15例(29%)报告2级纤维化,7例(14%)报告2级毛细血管扩张,1例报告3级毛细血管扩张;只有1例报告2级放射性皮炎。3例患者出现心律失常,需要有效的抗凝治疗。这些患者中有2例是右乳腺癌,1例是左乳腺癌。最后,一例被诊断甲状腺功能减退症。
41例(69%)患者行保乳手术(BCS), 18例患者行全乳房切除术,病理完全缓解率为27%(16/59例)。Berg I级和II级淋巴结清扫术切除了中位11个淋巴结(范围:3-23)。辅助治疗包括17%的患者仅接受FEC化疗,20%的患者仅接受内分泌治疗,51%的患者联合治疗。
13年的总生存率为70.9% (95%CI: 59.6-84.2)。20例患者死亡,其中17例死于乳腺癌。单因素分析显示组织学分级与总生存率相关(p = 0.01),同样被多因素分析证实(p = 0.04)。

总生存率
13年无转移生存率为71.5% (95%CI: 60.5-84.5),19例患者出现转移进展。4例患者发生第二种癌症(急性髓系白血病、卵巢癌、鳞状细胞癌和对乳腺癌的肺癌)。3例患者也发展为对侧浸润性乳腺癌。
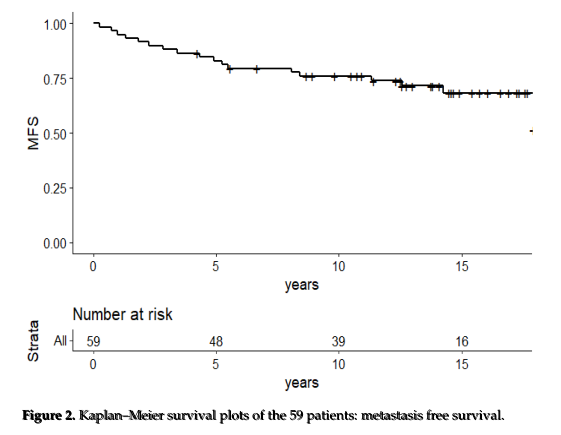
无转移生存率
局部区域控制率为83.4% (95%CI: 73.2-95.0)。2例乳房和区域复发,5例单独区域复发。所有局部复发都与转移进展相关,除了一个孤立的局部复发(腋窝和锁骨上复发通过局部手术、放疗和全身治疗,复发后13年病情稳定)。
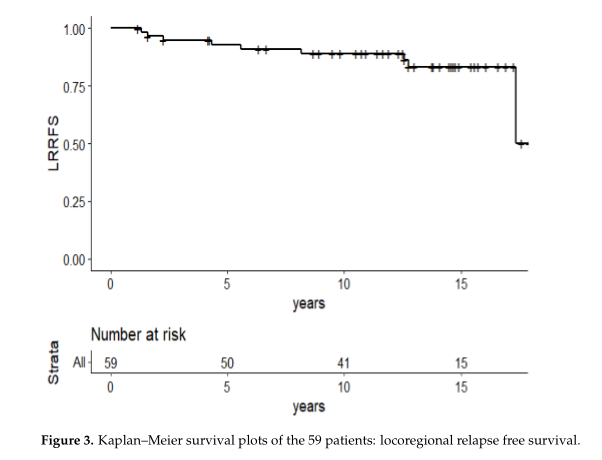
局部区域控制率
中位随访时间为13年(3-18),局部控制率为92.1% (95% CI: 83.7-100)。每个复发的病例都做了活组织检查。初始病变为1级、HR+、HER2-浸润性导管癌。
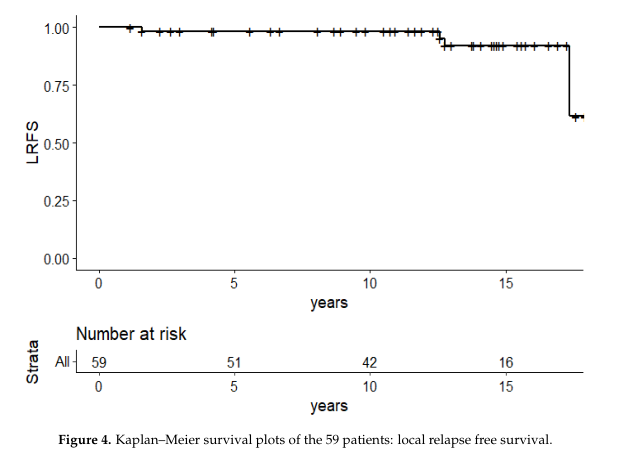
局部控制率
综上,研究表明,早期乳腺癌新辅助放化疗可取得较高的局部控制率以及有限的不良反应。
原始出处:
Jornet, D.; Loap, P.; Pierga, J.-Y.; Laki, F.; Vincent-Salomon, A.; Kirova, Y.M.; Fourquet, A. Neoadjuvant Concurrent Radiotherapy and Chemotherapy in Early Breast Cancer Patients: Long-Term Results of a Prospective Phase II Trial. Cancers 2021, 13, 5107. https://doi.org/10.3390/cancers13205107
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#辅助放化疗#
43
#新辅助#
40
#疗效和安全性#
30
#ERS#
30
#放化疗#
28
#新辅助放化疗#
33
#长期疗效#
34
#乳腺癌患者#
22
学习
49