培美曲塞是常用的抗肿瘤药物,常用于非鳞状非小细胞肺癌、恶性胸膜间皮瘤的治疗。本文总结了培美曲塞的作用机制、不良反应及其相关的预防用药和用药调整。
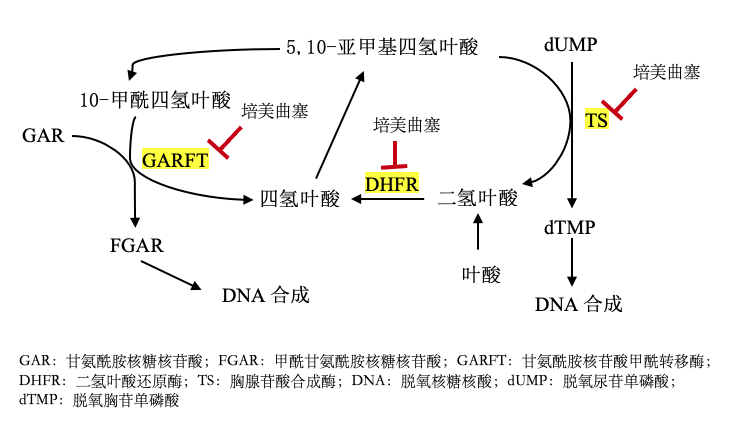
一、作用机制
-
ANC≥1500 cells/mm3
-
血小板计数≥100000 cells/mm3
-
CrCl≥45 ml/min
-
总胆红素≤1.5倍正常值上限
-
ALP、AST和ALT≤3倍正常值上限,或5倍正常值上限(肿瘤影响肝脏时可考虑)
-
ANC:绝对嗜中性粒细胞计数绝对值
-
CrCl:肌酐清除率
-
ALP:碱性磷酸酶
-
AST:天冬氨酸氨基转移酶
-
ALT:丙氨酸氨基转移酶
参考文献:
1. Lexicomp Online, Lexi-Drugs Online. Waltham,MA: UpToDate, Inc.; April 1, 2022. https://online.lexi.com. Accessed April 18, 2022.
2. 药物说明书, 培美曲塞二钠, AccessedApril 18, 2022.
3. Niyikiza C, Baker SD, Seitz DE, et al.Homocysteine and methylmalonic acid: markers to predict and avoid toxicity frompemetrexed therapy. Mol Cancer Ther. 2002;1(7):545-552.
4. Vogelzang NJ, Rusthoven JJ, Symanowski J, etal. Phase III study of pemetrexed in combination with cisplatin versuscisplatin alone in patients with malignant pleural mesothelioma. J ClinOncol. 2003;21(14):2636-2644. doi:10.1200/JCO.2003.11.136
5. Singh N, Baldi M, Kaur J, et al. Timing offolic acid/vitamin B12 supplementation and hematologic toxicity duringfirst-line treatment of patients with nonsquamous non-small cell lung cancerusing pemetrexed-based chemotherapy: The PEMVITASTART randomized trial. Cancer.2019;125(13):2203-2212. doi:10.1002/cncr.32028
6. Kim YS, Sun JM, Ahn JS, Ahn MJ, Park K. Theoptimal duration of vitamin supplementation prior to the first dose ofpemetrexed in patients with non-small-cell lung cancer. Lung Cancer.2013;81(2):231-235. doi:10.1016/j.lungcan.2013.04.011
7. Takagi Y, Hosomi Y, Sunami K, et al. Aprospective study of shortened vitamin supplementation prior tocisplatin-pemetrexed therapy for non-small cell lung cancer. Oncologist.2014;19(11):1194-1199. doi:10.1634/theoncologist.2014-0221
8. Schlei Z, Tan W, Faber MG, Chen H, Meagher A, Dy GK. Safetyof same-day vitamin B12 supplementation in patients receiving pemetrexed forthe treatment of non-small-cell lung cancer or pleural mesothelioma: aretrospective analysis. Clin Lung Cancer. 2018;19(6):467–75.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#同期#
40
#美曲塞#
42
***
44
#培美曲塞#
41
学习
59
感谢分享
42