NEJM:初诊稳定型胸痛,CT并不劣于侵入性冠状动脉造影!
2022-03-08 Nebula MedSci原创
稳定胸痛患者初始检查采用 CT 或 ICA 检查的主要心血管不良事件结局无明显差异。
侵入性冠状动脉造影 (ICA) 是诊断阻塞性冠状动脉疾病 (CAD) 的参考标准,可同时进行冠状动脉血运重建。但是,选择性 ICA 与罕见但主要的操作相关并发症相关;而且,据报道,只有38%至50%的进行 ICA 检查的患者有阻塞性冠状动脉疾病。
在阻塞性冠状动脉疾病的诊断中,计算机断层扫描 (CT) 是侵入性冠状动脉造影的一种准确、无创的替代检查。但是,CT 和 ICA 在管理 CAD 以降低主要心血管不良事件发生率方面的有效性孰高孰低尚不确定。
本研究是一项务实、随机化的临床试验,旨在对比 CT 和 ICA 作为指导具有中度阻塞性 CAD 可能的需进行 ICA 检查的稳定型胸痛患者的初步诊断影像学策略的有效性。主要终点是3.5年内的主要不良心血管事件(心源性死亡、非致命性心肌梗死或非致命性卒中)。次要终点包括与操作相关的并发症和心绞痛。
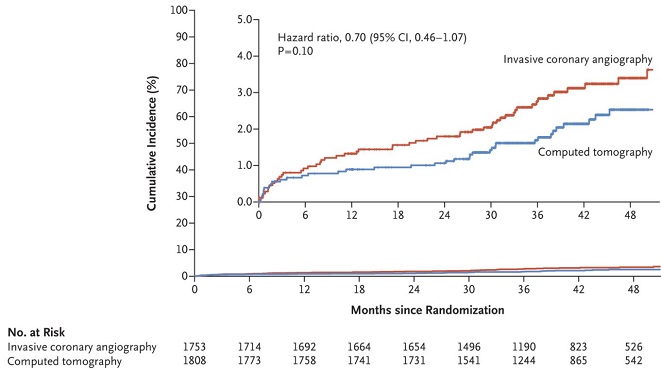
主要不良心血管事件的累积发生率
在3561位患者(56.2%的女性)中,3523位(98.9%)完成了随访,其中1808位在 CT 组,1753位在 ICA 组。CT 组和 ICA 组分别有2.1%和3.0%的患者发生了主要不良心血管事件(风险比 0.70,p=0.10)。CT 组有9位患者(0.5%)发生了主要的操作相关并发症,而ICA 组有33位(1.9%)发生了主要的操作相关并发症(风险比 0.26)。在随访的最后4周,CT 组有8.8%的患者、ICA 组有7.5%的患者报告了心绞痛(优势比 1.17)。
综上,对于因稳定胸痛和 CAD 中等预测概率而需进行 ICA 检查的患者中,初始检查采用 CT 或 ICA 对主要心血管不良事件风险的影响不分伯仲,但采用 CT 检查的患者的主要操作相关并发症的发生率较低。
原始出处:
The DISCHARGE Trial Group. CT or Invasive Coronary Angiography in Stable Chest Pain. NEJM. March 4, 2022. DOI: 10.1056/NEJMoa2200963.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#稳定型#
41
#侵入性#
58
#冠状动脉造影#
42
#造影#
52