PLoS ONE:发现头颈部鳞状细胞癌新的治疗靶点
2012-05-25 Deepblue 生物谷
近日,来自美国俄亥俄州立大学的研究人员发现,在头颈部鳞状细胞癌(HNSCC)细胞内,MicroRNA-34a的表达失调会促进了肿瘤的生长及肿瘤血管的生成,则控制miR-34a的活性也许能够成为新的策略来治疗HNSCC。相关研究成果于5月22日在线发表在PLoS ONE上。 MicroRNAs (miRs)是小的非编码RNA,在癌症发生过程中扮演了重要角色,研究发现,它们能够作为癌基因促进癌症发生

近日,来自美国俄亥俄州立大学的研究人员发现,在头颈部鳞状细胞癌(HNSCC)细胞内,MicroRNA-34a的表达失调会促进了肿瘤的生长及肿瘤血管的生成,则控制miR-34a的活性也许能够成为新的策略来治疗HNSCC。相关研究成果于5月22日在线发表在PLoS ONE上。
MicroRNAs (miRs)是小的非编码RNA,在癌症发生过程中扮演了重要角色,研究发现,它们能够作为癌基因促进癌症发生,也能够作为肿瘤抑制因子阻遏肿瘤的生成。miR-34a是一种肿瘤抑制因子,在一系列肿瘤类型中都被发现表达下调。然而,miR-34a对头颈部鳞状细胞癌(HNSCC)作用机制目前还不明确。
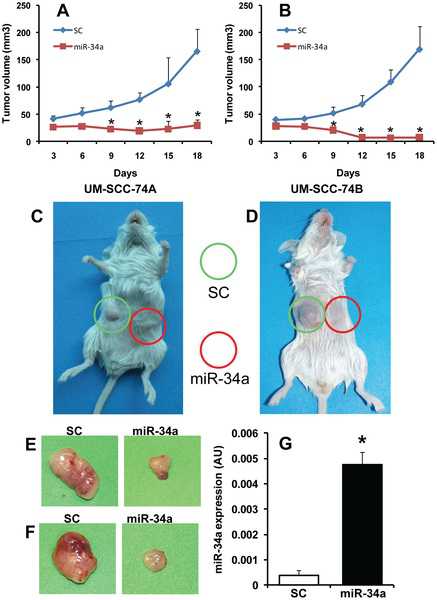
在这项研究里,研究人员发现,将miR-34a异位表达到HNSCC细胞系,能够显著的抑制肿瘤细胞的增生、集落形成以及细胞迁移。而且,过表达miR-34a也能够显著的下调E2F3以及生存素的水平。进一步研究发现,miR-34a介导的对细胞增生及集落形成的抑制作用,主要是通过E2F3a所介导。除此以外,对来自HNSCC患者的肿瘤样品的研究表明,miR-34a与生存素以及miR-34a与E2F3水平都表现出一个反相关的关系。
研究发现,在表达有miR-34a的细胞,E2F3a的过表达能够完全恢复生存素的表达水平,这表明miR-34a可能通过E2F3a调节了生存素的表达。在一个严重联合免疫缺陷(SCID)小鼠异种移植模型中,研究者还发现,miR-34a的异位表达也能够显著的抑制肿瘤的生长以及肿瘤血管生成。有趣的是,他们发现miR-34a是通过阻碍肿瘤细胞产生VEGF以及直接抑制内皮细胞的功能,来抑制肿瘤血管的生成。
该研究阐明了头颈部鳞状细胞癌(HNSCC)细胞内miR-34a的作用机制,Pawan Kumar表示,靶向一个miR-34a也许能够成为新的HNSCC治疗策略。

doi: 10.1371/journal.pone.00376
PMC:
PMID:
Dysregulation of MicroRNA-34a Expression in Head and Neck Squamous Cell Carcinoma Promotes Tumor Growth and Tumor Angiogenesis
Bhavna Kumar, Arti Yadav, James Lang, Theodoros N. Teknos, Pawan Kumar.
MicroRNAs (miRs) are small non-coding RNAs that play an important role in cancer development where they can act as oncogenes or as tumor-suppressors. miR-34a is a tumor-suppressor that is frequently downregulated in a number of tumor types. However, little is known about the role of miR-34a in head and neck squamous cell carcinoma (HNSCC).Ectopic expression of miR-34a in HNSCC cell lines significantly inhibited tumor cell proliferation, colony formation and migration. miR-34a overexpression also markedly downregulated E2F3 and survivin levels. Rescue experiments using microRNA resistant E2F3 isoforms suggest that miR-34a-mediated inhibition of cell proliferation and colony formation is predominantly mediated by E2F3a isoform. In addition, tumor samples from HNSCC patients showed an inverse relationship between miR-34a and survivin as well as miR-34a and E2F3 levels.Overexpression of E2F3a completely rescued survivin expression in miR-34a expressing cells, thereby suggesting that miR-34a may be regulating survivin expression via E2F3a. Ectopic expression of miR-34a also significantly inhibited tumor growth and tumor angiogenesis in a SCID mouse xenograft model. Interestingly, miR-34a inhibited tumor angiogenesis by blocking VEGF production by tumor cells as well as directly inhibiting endothelial cell functions.Taken together, these findings suggest that dysregulation of miR-34a expression is common in HNSCC and modulation of miR34a activity might represent a novel therapeutic strategy for the treatment of HNSCC.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#细胞癌#
27
#治疗靶点#
25
#Plos one#
26
#头颈部鳞状细胞癌#
38
#头颈部#
32
#颈部#
36