Blood:Trib1通过调节Hoxa9的转录来促进AML进展
2020-08-10 MedSci原创 MedSci原创
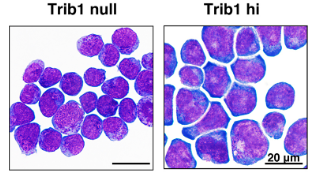
在髓系白血病发生过程中已观察到Trib1对Hoxa9的密切遗传作用,其中Trib1过表达可明显加速Hoxa9诱导的白血病发生。但Trib1如何功能性调节Hoxa9转录活性的潜在机制尚不清楚。
中心点:
Trib1可通过降解C/EBPα和修饰与Hoxa9相关的超级增强子来影响髓样白血病发生中的Hoxa9;
Erg是Trib1和Hoxa9的关键靶标,对BRD4抑制有反应,并在白血病发生中起关键作用。
摘要:
假激酶Trib1充当髓样癌基因,将E3泛素连接酶COP1募集到C/EBPa上,并与MEK1相互作用以增强ERK磷酸化。在髓系白血病发生过程中已观察到Trib1对Hoxa9的密切遗传作用,其中Trib1过表达可明显加速Hoxa9诱导的白血病发生。但Trib1如何功能性调节Hoxa9转录活性的潜在机制尚不清楚。
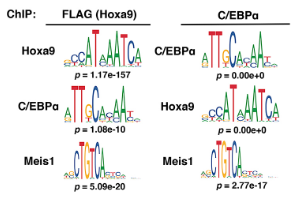
在本研究中,Yoshino等证实Trib1调节与Hoxa9相关的超级增强子。
ChIP-seq分析显示,Erg、Spns2、Rgl1和Pik3cd基因座的超级增强子处的组蛋白H3K27Ac信号增强,且伴随这些基因的mRNA表达增加。超级增强子活性的修饰主要通过Trib1降解C/EBPa p42来实现,而MEK/ERK通路的贡献较小。沉默Erg可消除Trib1过表达所获得的增长优势,表明Erg是Trib1 /Hoxa9轴的关键下游靶标。
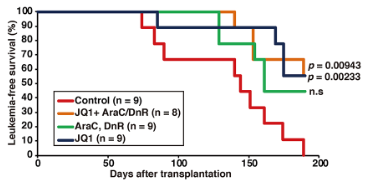
此外,用BRD4抑制剂JQ1治疗急性髓细胞性白血病(AML)细胞在体外和体内均表现为Trib1/Erg依赖性的生长抑制。在人AML细胞系中也观察到了TRIB1引起的ERG上调,提示Trib1是Hoxa9相关AML的潜在治疗靶标。
综上所述,该研究揭示了在髓样白血病发生过程中,Trib1调节染色质和Hoxa9驱动的转录的新机制。
原始出处:
Seiko Yoshino,et al. Trib1 promotes acute myeloid leukemia progression by modulating the transcriptional programs of Hoxa9. Blood. July 30, 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#转录#
31
#HoxA9#
22
学习
84
优秀
65