Clin Cancer Res:可预测晚期肝癌患者采用信迪利单抗+IBI305治疗预后的生物标志物
2022-04-05 xiaozeng MedSci原创 发表于威斯康星
血清CD137水平和肿瘤基质M1巨噬细胞密度可预测晚期肝癌患者采用信迪利单抗+IBI305治疗的预后
肝细胞癌(HCC)是最常见的恶性肿瘤之一,是全球癌症相关死亡的第三大原因。整体上,肝细胞癌的5年生存率只有5%-30%。抗血管生成药物(如索拉非尼、乐伐替尼等)是晚期肝细胞癌的标准系统治疗,但在进行标准系统治疗的情况下,肝细胞癌患者的中位总生存期也只有10.7-13.6个月。
本研究旨在探索抗PD-1抗体信迪利单抗联合贝伐单抗生物类似物IBI305治疗晚期肝细胞癌的疗效和安全性,以及相关生物标志物。
招募了50位18-75岁的晚期肝细胞癌患者,予以信迪利单抗(200 mg)+IBI305(7.5或15mg/kg)治疗,每3周一个疗程。主要终点是安全性,次要终点包括客观缓解率、疾病控制率、无进展生存期和总生存期。此外,研究人员还采用多重免疫测定和多重免疫荧光测定检测了基线肿瘤组织中的血清细胞因子,以探索与患者对研究治疗反应相关的生物标志物。
不良反应
截止2021年5月13日,有4位患者仍在接受治疗,中位治疗疗程是8个。总缓解率为34%(17/50)。中位无进展生存期和总生存期分别是10.5个月和20.2个月。7.5mg/kg剂量组的3-5级不良反应的发生率低于15mg/kg剂量组(13.8% vs 28.6%)。
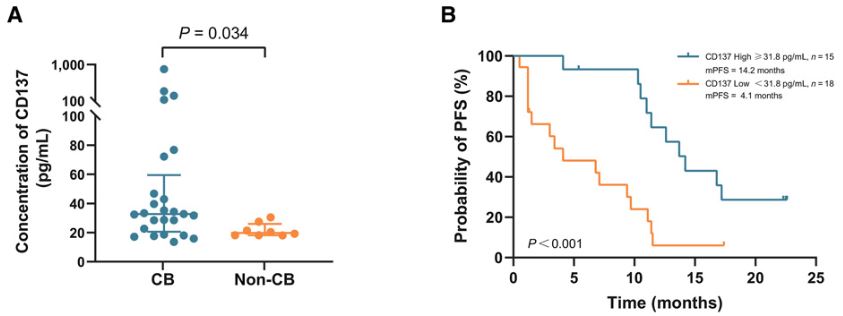
血清CD137水平不同的患者的无进展生存期
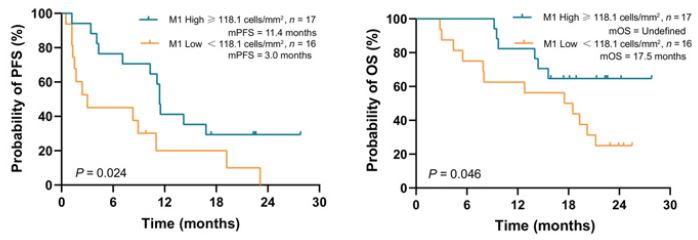
生物标志物分析显示,有临床获益(CB)的患者的血清CD137浓度显著高于没有临床获益的患者(中位值:32.8pg/ml vs 19.8pg/ml,p=0.034)。与CD137低水平的患者相比,CD137高水平患者的无进展生存期明显延长(中位值:14.2个月 vs 4.1个月,p=0.001)。此外,基质中较高的M1巨噬细胞(CD68+CD163-)密度也与更好的疗效(p=0.033)和更长的无进展生存期(p=0.024)相关。
肿瘤基质浸润M1巨噬细胞密度不同的患者的无进展生存期和总生存期
综上,该研究结果提示,信迪利单抗与IBI305的联合方案在晚期肝细胞癌患者中的耐受性良好,而且具有一定疗效。血清CD137水平和肿瘤基质M1巨噬细胞密度或均可作为潜在预测预后的生物标志物。
原始出处:
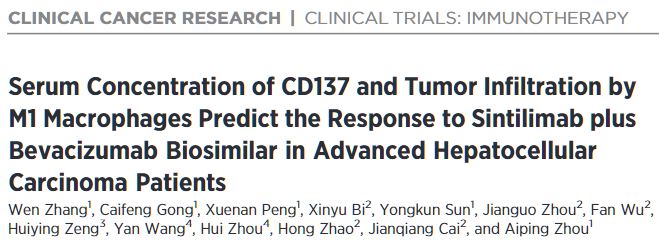
Wen Zhang, et al. Serum Concentration of CD137 and Tumor Infiltration by M1 Macrophages Predict the Response to Sintilimab plus Bevacizumab Biosimilar in Advanced Hepatocellular Carcinoma Patients. Clin Cancer Res OF1–OF10. https://doi.org/10.1158/1078-0432.CCR-21-3972
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#标志物#
43
#信迪利单抗#与#肝癌#
124
#肝癌患者#
45
#生物标志#
52
#生物标志#
38