PHILIPS每日一例:脾硬化性血管瘤样结节性转化的影像学表现2例
2022-09-13 放射沙龙 中华肝胆外科杂志
脾硬化性血管瘤样结节性转化,单发、无包膜和囊变坏死、伴有持续低密度或低信号的星芒状纤维瘢痕、以及特异的从动脉期到延迟期呈现逐渐向心性充填的“辐轮状”强化是SANT的影像学特点。
脾硬化性血管瘤样结节性转化(sclerosing angiomatoid nodular transformation,SANT)是近年才被认识的一种少见脾脏肿瘤,有关影像报道的文献少见。我们曾遇2例脾脏SANT,由于对本病的影像表现认识不足均导致误诊。现结合有关文献报道如下。
临床资料
例1、男,56岁。因右侧腹部隐痛4个月入院。患者无贫血、发热、恶心呕吐等不适。体格检查:腹平软,肝脾肋下未触及。右中上腹可触及7 cm大小质硬光滑不活动包块,无触痛及叩痛。
CT平扫加增强扫描提示右肾及脾占位。脾脏内类圆形稍低密度病灶大小约5.4 cm×5.0 cm,边界清楚;增强后动脉期可见边缘及分隔状强化,静脉期及延迟期逐渐向中心充填,密度趋于均匀并稍高于周围脾脏密度,中心呈持续低密度(图1~5)。
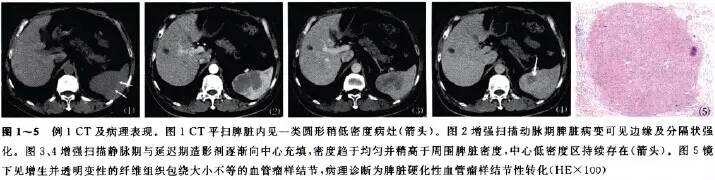
行根治性右肾切除、脾切除术。术后病理:右肾透明细胞癌,脾硬化性血管瘤样结节性转化。免疫组织化学检查:CD34(+)、CD31(+)、CD21(-)、CD35(-)、S-100(-)。
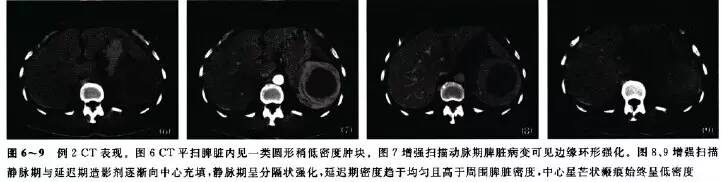
例2 、女,51岁。体检发现脾占位3年,体格检查及实验室检查无明显异常。CT平扫脾内见大小约7.5 cm×6.2 cm稍低密度肿块,边界较清楚;增强后动脉期肿块周边环形强化,静脉期呈分隔状强化,延迟期密度趋于均匀且高于周围脾脏密度,中央瘢痕始终呈低密度(图6~9)。
MRI见肿块状呈浅分叶,边界清楚。T1WI呈等信号,T2WI与脾相比呈稍低信号,中心见星芒状低信号。动脉期呈边缘及分隔状强化,门静脉期强化逐渐向中央推进而形成“辐轮状”强化,延迟期持续强化且信号高于周围脾实质,中央星芒状结构始终呈低信号(图10~15)。

术后病理:脾硬化性血管瘤样结节性转化。免疫组织化学检查:CD31(+)、CD34(+)、CD68(+)、SMA(-)、DES(-)、F8(+)、S-100(+)、ALK(-)。
讨论
脾硬化性血管瘤样结节性转化是一种少见的脾良性病变Ⅲ。SANT首先由Krishnan于1993年报道,原称脾索状毛细血管瘤(cord capillary hemangioma)。Rosai等在第9版《Rosai和Ackerman外科病理学》中把这种病变命名为多结节性血管瘤(multinodular hemangioma)。
直到2004年Martel等才根据其特征性的病理形态、免疫组化表型及良好的临床经过,提出该病变是脾内一种良性血管性病变,并正式将其命名为脾脏硬化性血管瘤样结节性转化。SANT患者多为女性,男女之比约1:2。
对该病变的发生机制目前还不清楚,Martel等认为SANT是一种包括炎性假瘤在内的各种脾损伤的终末病变。患者的临床症状和体征无特异性,部分患者是在体检时偶然发现。SANT可同时伴有其他疾病,如慢性淋巴细胞白血病、肺鳞癌、结肠癌、早期胃癌、肾癌等。
本文例1即以肾癌就诊,发现脾占位。本病预后良好,脾脏切除即可治愈。SANT通常为单发,与周围脾分界清楚,无包膜和囊变坏死,中心可见灰白色纤维瘢痕。SANT具有相对特征性的组织形态和免疫组化标志,纤维硬化间质中多个血管瘤样结节是本病变的组织学特征,其免疫组织化学存在CD34、CD31等血管阳性表达。
SANT在CT平扫时表现为边界清楚的稍低或低密度肿块,偶见报道有小钙化灶及出血时呈高密度。MRI平扫T1WI呈等或稍低信号,伴出血时其内可见高信号;T2WI相对于脾呈不均匀低信号。Li等首次详细报道了1例SANT的CT表现,平扫病变呈低密度伴小灶状钙化,门静脉早期开始强化,逐渐趋于均匀,随脾脏强化程度减低,至门静脉晚期肿块与周围脾实质呈等密度,分界不清。
本组例1术前考虑肾癌伴脾转移,术后明确为肾癌合并SANT。CT表现为动脉期边缘环形及分隔状强化,门静脉期逐渐向中心填充,延迟期病灶密度趋于均匀,伴持续的中心低密度区;该例脾脏SANT的CT增强表现与Zeeb等报道的一致。Karaosmanoglu及Thacker等报道SANT的MRI增强显示动脉期、门静脉期病变呈边缘环状强化和向中心的辐射状强化,这种形态学表现被认为是“辐轮状”强化。延迟期造影剂从病变边缘渐向中心充填,低信号的星芒状中心持续存在。病灶中央的低信号可能反映了纤维瘢痕组织和含铁血黄素沉着。
脾SANT的影像学表现与病理有一定的相关性。目前,SANT的CT和MRI均无坏死囊变的报道,增强扫描后病灶内常见非囊变坏死的低密度或低信号星芒状中心,结合本组2例以及SANT的病理学特点考虑可能主要是乏血管的瘢痕组织。从动脉期到延迟期呈现逐渐向心性充填的“辐轮状”强化,可能主要是被分隔的富血管的血管瘤样结节组织。
总之,单发、无包膜和囊变坏死、伴有持续低密度或低信号的星芒状纤维瘢痕、以及特异的从动脉期到延迟期呈现逐渐向心性充填的“辐轮状”强化是SANT的影像学特点。SANT是脾内一种具有特征性的的罕见良性病变,临床缺乏特异性,常不被临床和放射科医师认识。熟悉SANT的影像学表现,有助于更好的与脾的其他疾病相鉴别,但最终确诊仍依赖于病理组织学检查。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#结节性#
37
#脾硬化性#
43
#血管瘤#
60
#iPS#
43
#硬化性#
43