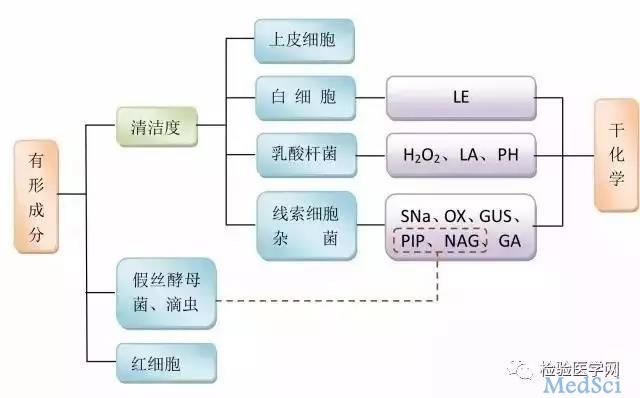
阴道分泌物检验的解读
2017-08-01 佚名 迪瑞医疗、检验医学网
女性的下生殖道为开放性腔道,是人体内一个重要的微生态系统,正常育龄女性阴道内有超过200种微生物,其中以乳酸杆菌为优势菌,超过95%的阴道菌都是乳酸杆菌,其余5%是条件致病菌及过路菌。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#分泌物#
50
#分泌#
36
#阴道分泌物#
51
学习了
64
很好,写的用心,看的舒心
69
学习了
71
受益了,谢谢分享……
68
学习了
70