癌症研究的最大挑战之一是如何防止已接受治疗的患者复发,复发的原因是某些癌细胞能够存活下来并生长成新的肿瘤。英国弗朗西斯·克里克研究所的研究人员发表在《Nature Communications》上的文章中,确定了一种临床上具有良好耐受性的药物,可以防止小鼠复发癌症。
https://doi.org/10.1038/s41467-020-15615-z
这种实验性药物名为Quisinostat,它通过增加肿瘤细胞内组蛋白H1.0的量来起作用,H1.0是一种抑制多种癌症类型癌细胞自我更新的肿瘤抑制因子。研究小组在小鼠的肿瘤中测试了该药物,发现它可以在对小鼠进行初步治疗后阻止肿瘤的再生长,并且,当对取自乳腺癌、肺癌或胰腺癌患者的细胞进行测试时,癌细胞被困在非分裂状态,药物阻止了存活的人类癌细胞在培养物中的扩增。
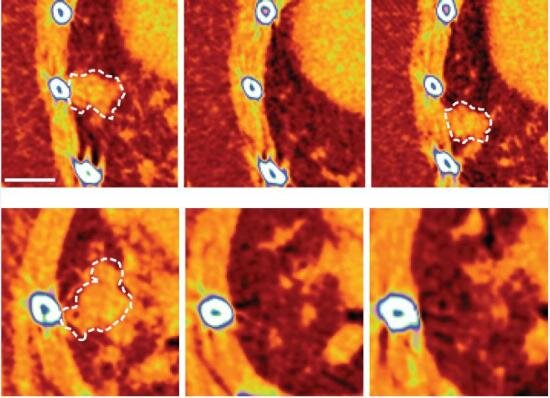
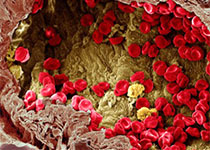
靶向治疗后小鼠肺肿瘤复发(上图),以及初始治疗后使用Quisinostat治疗的小鼠肺肿瘤无法生长(下图)。图片来源:弗朗西斯·克里克研究所
研究人员希望,如果在进一步的测试和临床试验中被证明有效,这种药物可用于治疗后的患者,以防止任何残留的癌细胞导致疾病复发。Quisinostat的作用是使那些促进癌症长期生长并导致疾病复发的细胞失去活性,在不同的患者、不同的癌症类型之间的差异可能会带来广泛的治疗益处,可能比常用的抑制肿瘤生长的药物更有效。重要的是,这项早期工作还表明Quisionostat可以影响癌细胞,而不会损害健康细胞。
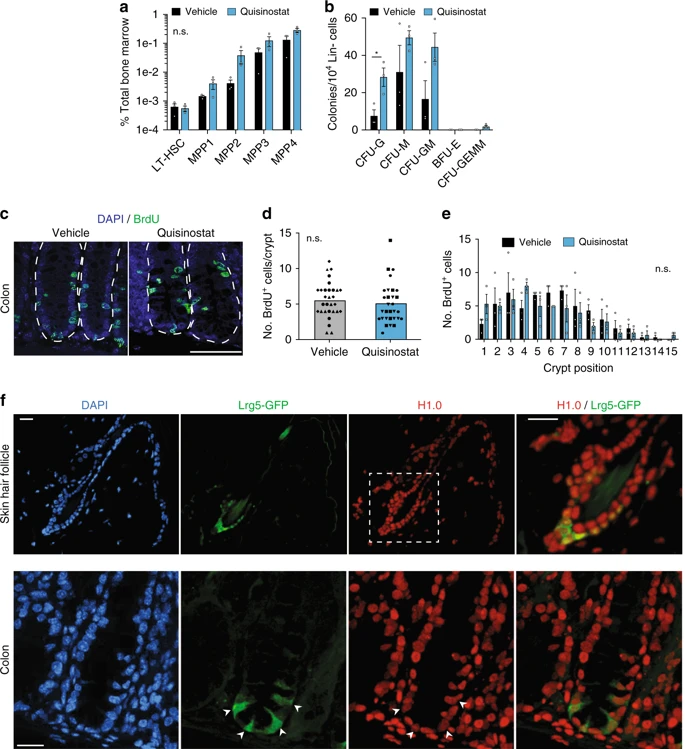
Quisinostat治疗不会损害正常的组织干细胞功能。
研究人员的下一步计划将是了解为什么Quisinostat对健康和恶性细胞具有不同的作用,以及组蛋白H1.0是否能告诉我们是什么使癌细胞区别于干细胞。
原始出处:
Morales Torres, C., Wu, M.Y., Hobor, S. et al. Selective inhibition of cancer cell self-renewal through a Quisinostat-histone H1.0 axis. Nat Commun 11, 1792 (2020). https://doi.org/10.1038/s41467-020-15615-z.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#COMMUN#
34
#Nat#
32
#实验性#
27
#癌症复发#
40
#防癌#
43