JACC:世界首例经导管实施三尖瓣修复手术
2015-03-09 赵洲译 MedSci原创
许多研究表明严重的三尖瓣反流与不良预后有关。然而,只有有限的1类适应症可以进行治疗,而高手术风险的病人则无法治愈。来自德国等地的研究人员报道了世界上首例成功的经导管三尖瓣修复手术用于治疗严重的三尖瓣反流。 一位89岁的妇女接受了此次手术。她患有复发性的右心代偿失调,表现为严重的下肢水肿和皮肤溃疡,并患有3-4期的慢性肾病以及慢性房颤。超声心动图和血液动力学的研究一致表明其患有三尖瓣反流。患者的心

许多研究表明严重的三尖瓣反流与不良预后有关。然而,只有有限的1类适应症可以进行治疗,而高手术风险的病人则无法治愈。来自德国等地的研究人员报道了世界上首例成功的经导管三尖瓣修复手术用于治疗严重的三尖瓣反流。
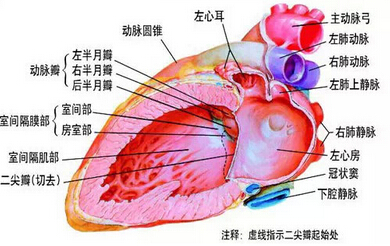
一位89岁的妇女接受了此次手术。她患有复发性的右心代偿失调,表现为严重的下肢水肿和皮肤溃疡,并患有3-4期的慢性肾病以及慢性房颤。超声心动图和血液动力学的研究一致表明其患有三尖瓣反流。患者的心脏手术风险评估指数(Lof EuroSCORE)为28%,手术治疗被认为有着过高的风险。但她同意了接受三尖瓣修复手术。
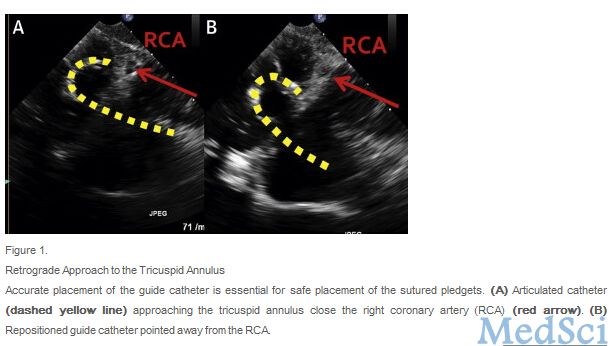
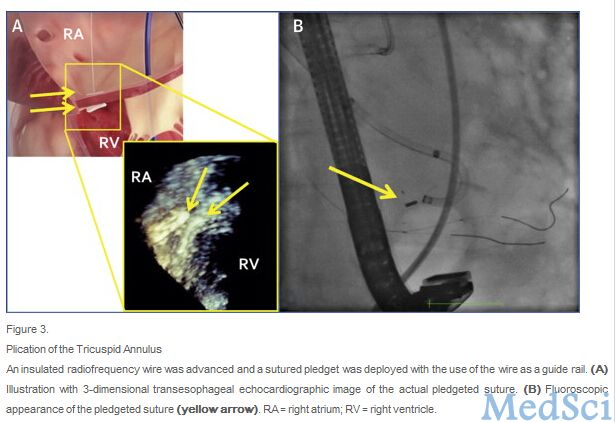
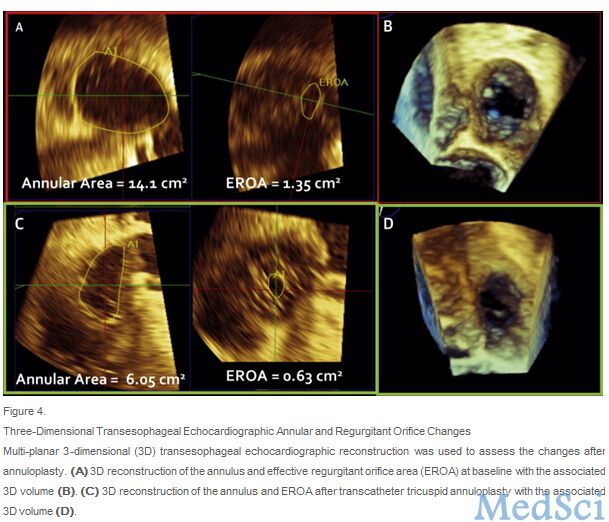
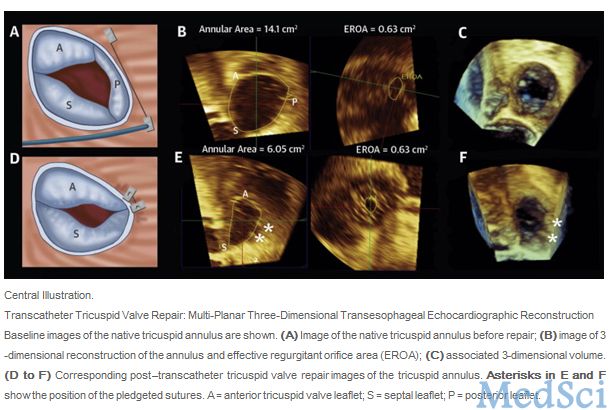
手术中对患者进行全麻,使用2D和3D经食道超声心动图进行监测。手术结果表明环状区域面积有着明显的减少(57%)。血流动力学监测也表明右心房压力从基线的22mmHg降低到9mmHg,左心室心搏量从基线时的42ml上升到72ml。病人很好地承受住了手术,并且在手术结束后当天拔掉了插管,5天后就出院了。出院后,病人继续接受日常的药物治疗。但是,她主观上感觉更好受,其下肢水肿已经减弱了,肾功能叶明显地得到了改善。
当然,这一研究仍有局限性。此次报道仅仅是一件治疗案例。这一案例表现出了经导管三尖瓣修复手术一定的可行性。但仍需要更多的病人对这一治疗方案的可行性和有效性进行评估。
原始出处:
Joachim Schofer, MD, Klaudija Bijuklic, MD, Claudia Tiburtius, MD, Lorenz Hansen, MD, Adam Groothuis, PhD, Rebecca T. Hahn, MD.First-in-Human Transcatheter Tricuspid Valve Repair in a Patient With Severely Regurgitant Tricuspid Valve.JACC.Available online 4 March 2015
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#世界首例#
35
#JACC#
44
希望这个方法能具体广泛应用
121
不错的课程
104
#ACC#
25
#经导管#
37
#三尖瓣#
39
怎么修复的?
98