Braz J Otorhinolaryngol:刮除式腺样体切除术与内镜辅助下微创腺样体切除术在耳咽管功能障碍方面的比较
2020-06-19 MedSci原创 MedSci原创
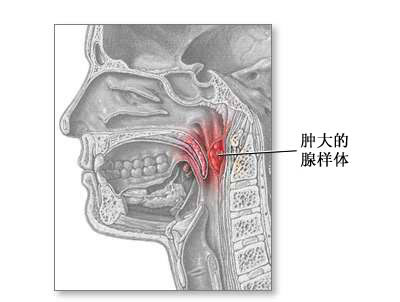
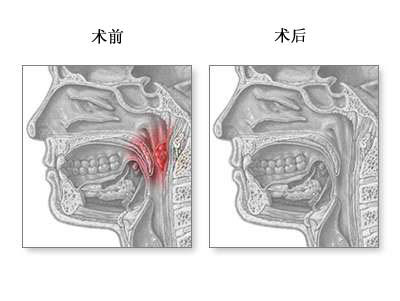
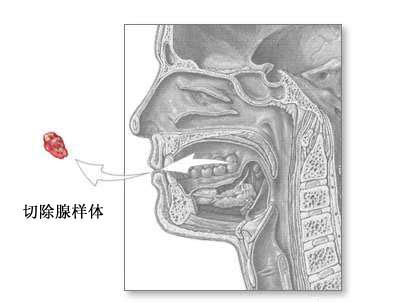
腺样体切除术可以通过多种方式进行,包括刮除术和微清器内镜辅助腺样体切除术。这两种技术各有利弊。本研究旨在探究刮除腺样体切除术和内镜辅助微清创性腺样体切除术对小儿腺样体肥大而无渗出性中耳炎的小儿鼓室压力
腺样体切除术可以通过多种方式进行,包括刮除术和微清器内镜辅助腺样体切除术。这两种技术各有利弊。本研究旨在探究刮除腺样体切除术和内镜辅助微清创性腺样体切除术对小儿腺样体肥大而无渗出性中耳炎的小儿鼓室压力的影响。
这项前瞻性描述性研究是对65名鼓膜正常且鼓室图正常,然后接受腺样体切除术或腺扁桃体切除术治疗腺样体和扁桃体肥大的患者进行的。将受试者随机分为两组:刮除腺样体切除术组和内镜微清创术辅助腺样体切除术组。他们进行了鼓室测压,并比较了术前和术后第1天和术后第7天的鼓室压力值。
结果,刮除腺样体切除术组32例,微清创性腺样体切除术组33例。刮除腺样体切除术的左耳和右耳在术前,术后第1天和术后第7天的鼓膜中位压力存在统计学差异(p <0.001,p <0.001)。这种差异发生在术后第一天,并且在第七天恢复到正常值。在微清创性腺样体切除术组中,左耳和右耳的术前,术后第1天和术后第7天的中鼓膜压力无显着差异(p = 0.376,p = 0.128)。
总之,该研究结果表明,与传统的腺样体切除术相比,内镜辅助微清创器腺样体切除术较少见术后咽鼓管功能障碍。
原始出处:
Mahmut Huntürk Atilla, Selda Kargın Kaytez, et al., Comparison Between Curettage Adenoidectomy and Endoscopic-Assisted Microdebrider Adenoidectomy in Terms of Eustachian Tube Dysfunction. Braz J Otorhinolaryngol. Jan-Feb 2020;86(1):38-43. doi: 10.1016/j.bjorl.2018.08.004. Epub 2018 Sep 25.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#AZ#
35
#腺样体切除术#
28
#切除术#
21
#内镜#
20
#微创#
22
#功能障碍#
23