Lancet Oncol:受试者自行采样HPV测试或为宫颈癌常规筛查项目
2014-02-10 佚名 www.thelancet.com
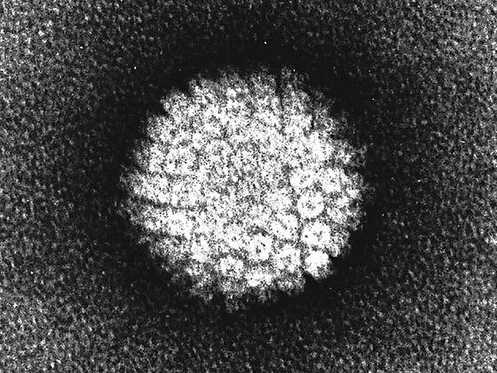
与宫颈涂片检查相比,人类乳头状瘤病毒(HPV)感染的筛查测试在降低宫颈癌发病率方面更有效。此外,HPV测试能经由女性自行采集阴道标本,因此可以改善该项检查的覆盖率。然而,HPV自行取样检测的结果精确性目前还不甚明确。【原文下载】 在本研究中,来自于比利时公共卫生科学研究所的Marc Arbyn等为了评估自行采样的HPV测试样本对测试准确性的影响是否与临床医师采样相
与宫颈涂片检查相比,人类乳头状瘤病毒(HPV)感染的筛查测试在降低宫颈癌发病率方面更有效。此外,HPV测试能经由女性自行采集阴道标本,因此可以改善该项检查的覆盖率。然而,HPV自行取样检测的结果精确性目前还不甚明确。【原文下载】
在本研究中,来自于比利时公共卫生科学研究所的Marc Arbyn等为了评估自行采样的HPV测试样本对测试准确性的影响是否与临床医师采样相等,因此他们进行了荟萃分析,并将研究结果发表在Lancet Oncol 2014年1月的在线期刊上。
研究者首先通过检索PubMed、Embase和CENTRAL找到相关的研究。研究者最后纳入荟萃分析的研究需满足以下标准:首先由女性受试者采取宫颈细胞的标本,其次由临床医师采样;对患者自行采集的标本进行高危HPV测试,对由临床医师采集的标本进行HPV测试或细胞学检测;在所有的女性受试者或既往检查为阳性的女性受试者中,如果缺乏或存在宫颈上皮内瘤样病变2级(CIN2)或以上,则需要进一步进行阴道镜检查和活检。
研究者采用二元正态模型和随机效应模型来确定发现CIN2或以上、CIN3或以上状态的绝对精确性,以及检测出上述状态的相对精确性。
研究者共纳入了36个研究,这些研究中共纳入了154556名女性患者。不同临床情况下的绝对精确性存在差异。在筛查中,自行采样的HPV检测对CIN2的平均检出率为76%,对CIN3的平均检出率为86%.而排除CIN2和CIN3的绝对特异性分别为86%和87%.由于对自我采样结果和临床医师采样结果进行比较所得的HPV测试的相对准确性较低,因此需对所有研究的结果进行汇集来评估相对准确性。
在汇集分析中,自我采样HPV检测的敏感性仍低于临床医师采样的HPV测试,检测出CIN2和CIN3的HR分别为0.88和0.89.同样,自我采样的测试结果的特异性也低于临床医师采样的测试结果,检测出CIN2和CIN3的HR分别为0.96和0.96.在HPV测试中,患者自我采样的敏感性和特异性都低于临床医师采样。与之相对,在一些基于PCR的HPV测试中,患者自我采样的敏感性和特异性都与临床医师采样的结果相似。
本研究结果指出,应用基于信号序列的筛查项目中,推荐由临床医师采集检测所需要的样本。然而,对于没有纳入常规筛查项目中的女性而言,建议采用自我采样来进行HPV测试。在仔细评估实施的可行、受试者依从性和检测成本之后,可将一些基于PCR的HPV检测作为常规筛查项目。
研究背景
由于高危类型的人类乳头状瘤病毒持续感染和宫颈癌发病之间存在极强的联系,因此需要找到合适的序列来检测出上述病毒的核苷酸序列。荟萃分析结果提供的临床证据促使临床应用HPV测试对模棱两可的细胞学检查进行辨别,以及用于预测宫颈癌前病变在治疗后的复发情况。
来自于随机对照研究的数据提示与既往巴氏涂片检查结果阴性的女性相比,既往HPV测试结果阴性的女性出现CIN3和侵袭性宫颈癌的风险更低。这一新的证据提示要改变宫颈癌的二级预防策略,应将HPV测试作为首要的筛查测试,可以作为代替巴氏涂片的检查方案或与巴氏涂片检查联合进行。此外,HPV测试能由女性受试者自行通过阴道采样,这可以适用于不愿意进行妇科检查的女性。
既往的荟萃分析总结了自行采样的受试者进行HPV测试结果的准确性和特异性等指标,但是这些综述的进行时间为6-8年之前,并且包含的是主要是小样本的研究,其评价的仅为病毒学结果,或是没有比较与临床医师采样所得到的结果在评价高级别的CIN方面的准确性。一项综述的结果提示需要大样本的研究提供更多的数据。
在本系统综述中,研究者评价了受试者自行采样所得到的标本的HPV测试用于确定高级别CIN或肿瘤的精确性。此外,研究者也比较了受试者自行采样所进行的HPV测试的结果和由临床医师采样所进行的细胞学检查的结果的差异。研究者没有比较由受试者自行采样所进行的细胞学测试的结果是因为既往的研究已经证实这种检测方法对于辨别高级别CIN病变的敏感性较差。
研究者关注于宫颈癌筛查的主要方法,因为由受试者自行采样是最常用的方法,以及在由于存在宫颈异常病变而进行随访的女性受试者中该测试的绝对准确性可能存在不同。在本荟萃分析中,研究者的目的在于确定由患者自行采样的HPV测试的结果和由临床医师采样所进行的HPV测试结果对在宫颈肿瘤筛查方面的价值是否相同。
原始出处:
Arbyn M1, Verdoodt F2, Snijders PJ3, Verhoef VM3, Suonio E4, Dillner L5, Minozzi S6, Bellisario C6, Banzi R7, Zhao FH8, Hillemanns P9, Anttila A10.Accuracy of human papillomavirus testing on self-collected versus clinician-collected samples: a meta-analysis.Lancet Oncol. 2014 Feb;15(2):172-83. doi: 10.1016/S1470-2045(13)70570-9. Epub 2014 Jan 14.【原文下载】
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Lancet#
28
#Oncol#
27
#筛查项目#
28
#宫颈#
32
#受试者#
22