Clin Cancer Res:采用抗CCR4单抗Mogamulizumab联合纳武单抗治疗局部晚期或转移性实体瘤
2021-11-18 Nebula MedSci原创
Mogamulizumab是一种靶向效应调节T细胞(eTreg)的抗CCR4单克隆抗体
程序性细胞死亡-1 (PD-1) 是一种通常在恶性肿瘤细胞上表达的调节受体,通过下调T细胞和B细胞的激活,帮助肿瘤细胞实现免疫逃逸。目前使用纳武单抗和派姆单抗等药物进行PD-1抑制免疫治疗,已被公认为癌症治疗的重大进展。
Mogamulizumab是一种靶向效应调节T细胞(eTreg)的抗CCR4单克隆抗体。该研究旨在明确Mogamulizumab联合检查点抑制剂纳武单抗在局部晚期或转移性实体瘤中的安全性、抗肿瘤活性和药效学。
这是一项多中心、剂量探索性(I期)和剂量扩展性(II期)研究,招募了局部晚期或转移性实体瘤患者。I期试验剂量是:在第1疗程中,Mogamulizumab 1mg/kg·周,随后改为1 mg/kg·2周,加上纳武单抗 240 mg/2周。在I期试验过程中,未发生剂量限制性毒性,因此,在2期扩展阶段继续采用该剂量水平。
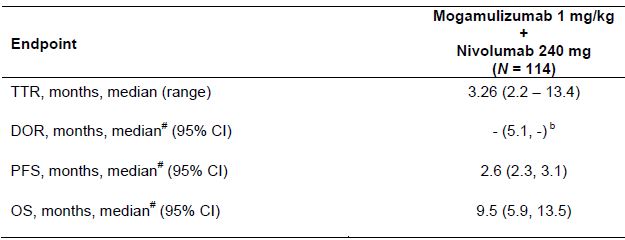
缓解前时间(TTR)、缓解持续时间(DOR)、无进展生存期(PFS)和总生存期(OS)
共114位患者接受了Mogamulizumab(1mg/kg)+纳武单抗(240 mg)治疗,其中4位在I期阶段,110位在II期阶段,均被纳入了安全性和有效性分析。Mogamulizumab联合纳武单抗显示出了可接受的安全性和耐受性。客观缓解率达到了10.5%(95% CI 5.6-17.7%),包括3例完全缓解和9例部分缓解。疾病控制率为36.8%。缓解持续时间为14.4个月。中位无进展生存期为2.6个月(95% CI 2.3-3.1),中位总生存期为9.5个月(5.9-13.5)。
综上,Mogamulizumab与纳武单抗联合治疗并未能提高局部晚期或转移性实体瘤的治疗效果。Mogamulizumab 1 mg/kg和纳武单抗 240 mg的联合方案的耐受性良好。
原始出处:
David S. Hong, Olivier Rixe, Vi K. Chiu, et al. Mogamulizumab in Combination with Nivolumab in a Phase I/II Study of Patients with Locally Advanced or Metastatic Solid Tumors. Clin Cancer Res November 9 2021 DOI:10.1158/1078-0432.CCR-21-2781
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#Mogamulizumab#
30
#局部晚期#
33
#mAb#
29
#转移性#
39
#局部#
28
#MOG#
35