Eur J Clin Pharmacol:DOAC剂量处方不当在≥80岁房颤患者中的发生率和预测因素分析
2022-02-16 “心关注”公众号 “心关注”公众号
对于符合口服抗凝治疗条件的房颤(AF)患者,直接口服抗凝剂(DOACs)通常比维生素拮抗剂(VKAs)更适合用于卒中预防,这基于良好的风险-获益评估,与患者年龄无关。尤其是在临床试验和真实世界数据中,
对于符合口服抗凝治疗条件的房颤(AF)患者,直接口服抗凝剂(DOACs)通常比维生素拮抗剂(VKAs)更适合用于卒中预防,这基于良好的风险-获益评估,与患者年龄无关。尤其是在临床试验和真实世界数据中,DOACs在≥80岁的超高龄AF患者中显示出比VKAs更高的临床净获益。然而,多达15%的AF患者DOACs处方中剂量可能不适当,其中高龄与DOACs处方剂量不当相关。
目前,关于老年患者DOACs处方剂量不当的临床数据有限,包括剂量不足和剂量过量。因此,本研究通过分析≥80岁老年群体的DOACs处方剂量特征,以描述DOACs处方剂量不当的发生率及与之相关的临床预测因素。
研究方法
本研究的数据来源于意大利三个医学中心前瞻性维护的AF数据库,共纳入253例年龄≥80岁并接受DOACs治疗的AF患者。所有受试者被分为标准剂量、剂量过量和剂量不足组。剂量不足和剂量过量分别定义为低于或高于欧洲心律协会(EHRA)共识建议的DOACs处方剂量。
主要终点是评估DOACs处方剂量不当的发生率,并描述研究人群中与处方剂量不当相关的临床因素。次要终点是确定DOACs标准剂量和剂量不当组的血栓栓塞事件(卒中、短暂性脑缺血发作[TIA]和体循环栓塞[SE]的复合终点)、大出血和死亡的发生率。
研究结果
所有患者的人口学和临床特征见表1。178例(71%)患者接受了标准剂量的DOACs处方;75例(29%)患者接受了剂量不当的DOACs处方,其中19例(25.60%)剂量过量,56例(74.40%)剂量不足。总体人群的CHA2DS2-VASc评分为4.50(±1.20)分,而HAS-BLED评分为2.90±0.90分。与标准剂量组相比,剂量不当组患者出现永久性AF(44% vs. 65%;P<0.001)及乙酰水杨酸联合用药(4% vs. 15.70%;P=0.009)的比例更低。
表1. 基线特征和临床结局

在多因素logistic回归分析中,较低的永久性AF发生率(OR 0.45,95%CI 0.22-0.91;P=0.03),联合使用低剂量乙酰水杨酸(OR 0.19,95%CI 0.05-0.71;P=0.01)与DOAC处方剂量不当独立相关(表2)。剂量不足与男性(OR 3.15,95%CI 1.45-6.83;P<0.001)、冠状动脉疾病(OR 3.60,95%CI 1.41-9.10;P<0.001)和BMI(OR 1.27,95%CI 1.14-1.41;P<0.001)独立相关。剂量过量与年龄(OR 0.76,95%CI 0.61-0.96;P=0.045),男性(OR 0.79,95%CI 0.05-0.84;P=0.021),糖尿病(OR 18,95%CI 3.36-96;P<0.001),BMI(OR 0.77,95%CI 0.62-0.97;P=0.04)和既往出血病史(OR 6.40,95%CI 1.43-28;P=0.03)独立相关。(表3,图1)
表2. 患者临床特征与DOACs剂量使用不当之间的关系
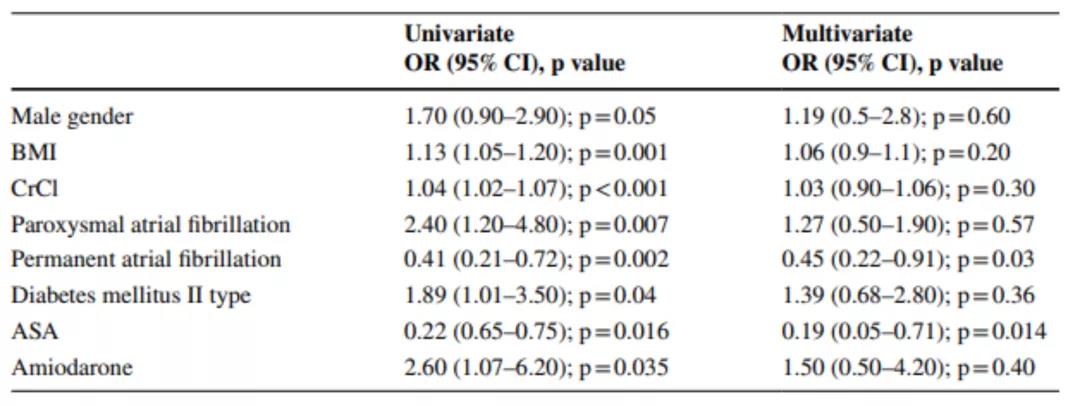
表3. 研究人群中DOAC剂量不足和过量的临床预测因素


图1. 森林图显示男性、CAD、DM II和BMI与DOAC过量和/或剂量不足风险的相关性
平均随访时间为32±10个月,共有46例患者(标准剂量组31例,剂量不当组15例)死亡;各组间无统计学差异。图2分别显示了各组的Kaplan-Meier累积生存率(P=0.004)。剂量不足组与标准剂量组相比,生存期明显降低(P<0.001)。
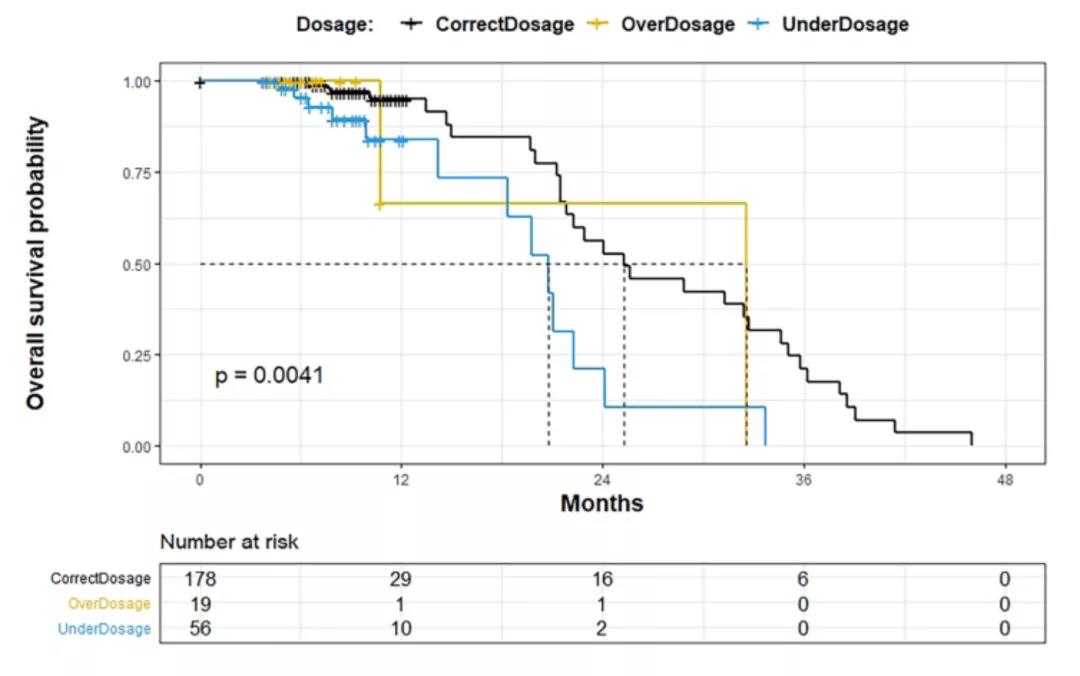
图2. Kaplan-Meier曲线比较适当剂量、过量和不足剂量DOACs亚组的存活率
在随访期间,12例患者(标准剂量组7例,剂量不当组5例;P=0.3)发生大出血事件;9例患者(标准剂量组7例,剂量不当组2例;P=0.6)发生血栓栓塞事件。三组患者的亚组分析显示,组间血栓栓塞和大出血事件均无显着差异。
多因素回归分析显示,男性(OR 2.10,95%CI 1.08-4.20;P=0.02),BMI<18.50 kg/m2(OR 5,95%CI -21-1.20;P=0.02)和SE/TIA(OR 4,95%CI 1.01-17;P=0.048)与死亡独立相关。
研究结论
在本分析中,近三分之一≥80岁的AF患者在进行DOACs治疗时,出现处方剂量不当的情况。合并糖尿病和有出血病史的患者服用过量药物的风险增加,而年龄、男性和较高的BMI与此呈负相关。此外,患有冠状动脉疾病和BMI较高的男性接受剂量不足处方的风险增加。剂量不足组的生存率明显低于标准剂量组。因此,对临床干预的进一步研究有助于解决老年患者DOACs处方剂量不当的情况。
原始出处:
Carbone A, Santelli F, Bottino R, et al. Prevalence and clinical predictors of inappropriate direct oral anticoagulant dosage in octagenarians with atrial fibrillation. Eur J Clin Pharmacol. 2022 Feb 9. doi: 10.1007/s00228-022-03286-2. Epub ahead of print. PMID: 35138442.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#Pharmacol#
41
#pharma#
38
#MAC#
48
#Pharm#
41
#发生率#
55
#预测因素#
40
#房颤患者#
54
因此,COVID-19患者应特别注意心脏
51
厉害
55