Cell Metab:日研究阐明非酒精性脂肪肝发病机制
2012-07-06 蓝建中 新华网
7月4日,日本横滨市立大学和大阪大学的联合研究小组宣布,他们首次弄清了非酒精性脂肪肝的发病机制。他们确认,一些肥胖者的肝脏会与肠内的细菌发生过敏反应,从而导致肝部发病。 非酒精性脂肪肝多由肥胖引起。它是指患者无饮酒史,但病理学上和酒精性脂肪肝患者有相似的病理状态,比如也有肝细胞脂肪变性、肝小叶炎症,有时也有“酒精”玻璃样变性和肝纤维化等。 研究人员在动物实验中发现,实验鼠肥胖后,脂肪细胞大量分

7月4日,日本横滨市立大学和大阪大学的联合研究小组宣布,他们首次弄清了非酒精性脂肪肝的发病机制。他们确认,一些肥胖者的肝脏会与肠内的细菌发生过敏反应,从而导致肝部发病。
非酒精性脂肪肝多由肥胖引起。它是指患者无饮酒史,但病理学上和酒精性脂肪肝患者有相似的病理状态,比如也有肝细胞脂肪变性、肝小叶炎症,有时也有“酒精”玻璃样变性和肝纤维化等。
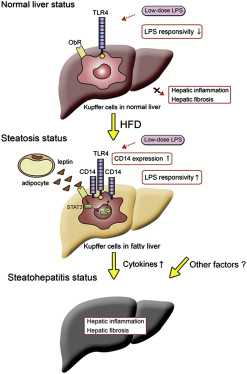
研究人员在动物实验中发现,实验鼠肥胖后,脂肪细胞大量分泌的肥胖基因编码产物Leptin会发挥作用,促使肝脏对肠内细菌分泌的毒素脂多糖发生过敏反应,从而导致肝部疾病。
横滨市立大学教授中岛淳说:“如同花粉症患者一样,肥胖者会对细菌发生过敏反应,这一发现将有助于开发新的诊疗方法。”相关论文已经刊登在美国《细胞—代谢》(Cell Metabolism)杂志网络版上。

doi:10.1016/j.cmet.2012.05.012
PMC:
PMID:
Hyperresponsivity to Low-Dose Endotoxin during Progression to Nonalcoholic Steatohepatitis Is Regulated by Leptin-Mediated Signaling
Kento Imajo, Koji Fujita, Masato Yoneda, Yuichi Nozaki, Yuji Ogawa, Yoshiyasu Shinohara, Shingo Kato, Hironori Mawatari, Wataru Shibata, Hiroshi Kitani, Kenichi Ikejima, Hiroyuki Kirikoshi, Noriko Nakajima, Satoru Saito, Shiro Maeyama, Sumio Watanabe, Koichiro Wada, Atsushi Nakajima
Although bacterial endotoxin, such as lipopolysaccharide (LPS), plays a key role in the pathogenesis of nonalcoholic steatohepatitis (NASH), detailed mechanisms of this pathogenesis remain unclear. Here, we demonstrate that upregulation of CD14 by leptin-mediated signaling is critical to hyperreactivity against endotoxin during NASH progression. Upregulation of CD14 in Kupffer cells and hyperreactivity against low-dose LPS were observed in high-fat diet (HFD)-induced steatosis mice, but not chow-fed-control mice. Hyperresponsivity against low-dose LPS led to accelerated NASH progression, including liver inflammation and fibrosis. Administering leptin in chow-fed mice caused increased hepatic expression of CD14 via STAT3 signaling, resulting in hyperreactivity against low-dose LPS without steatosis. In contrast, a marked decrease in hepatic CD14 expression was observed in leptin-deficient ob/ob mice, despite severe steatosis. Our results indicate that obesity-induced leptin plays a crucial role in NASH progression via enhanced responsivity to endotoxin, and we propose a mechanism of bacteria-mediated progression of NASH.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#非酒精性#
26
#酒精性脂肪肝#
40
#酒精性#
34
#CEL#
25
#Cell#
29
#MET#
21
#Meta#
23