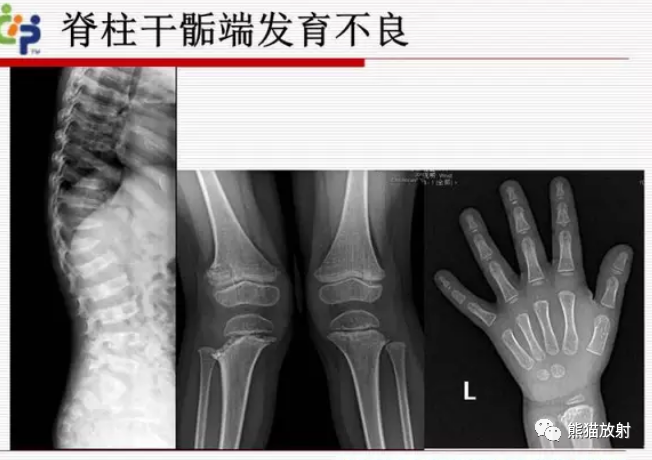
软骨发育不全的诊断要点是什么?
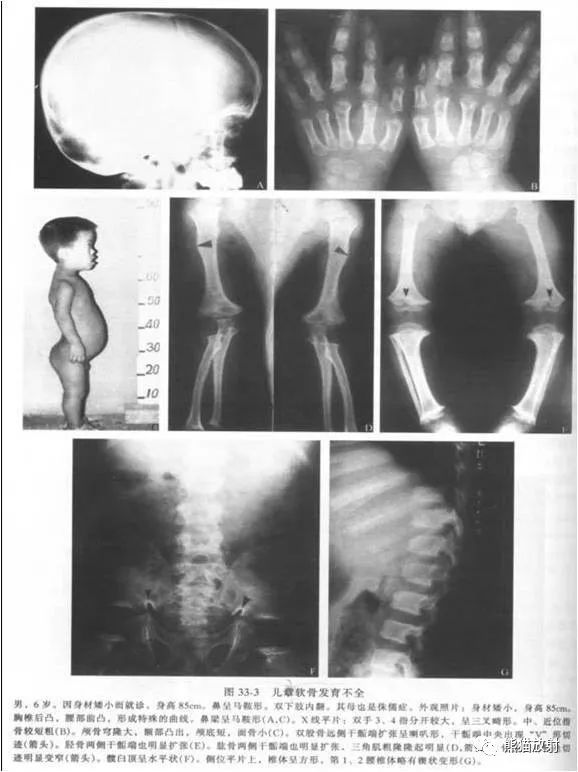
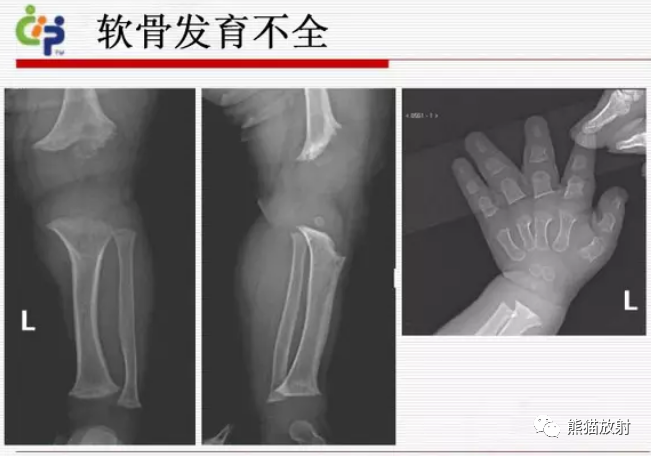
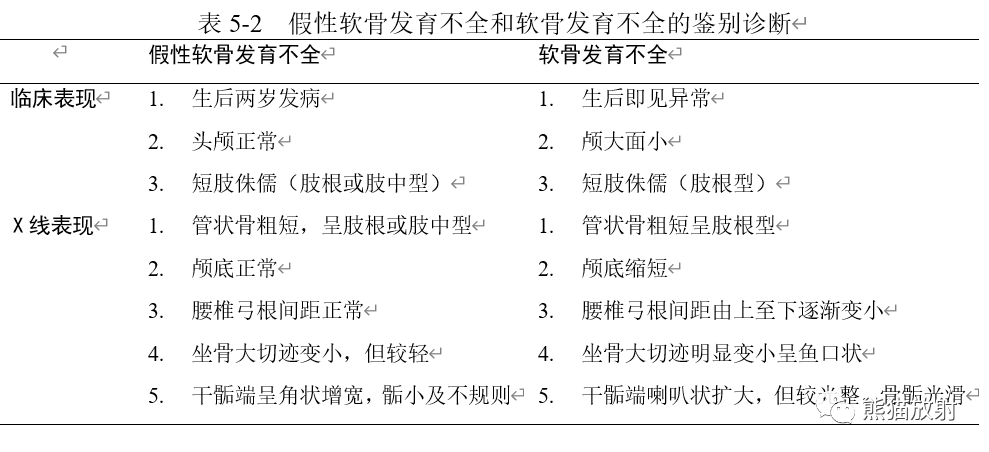
①长管骨粗短弯曲,干骺端增宽呈“杯口”或“V”型,骨骺被其包埋,以膝部表现为显著。骺板光滑或轻度不整(是与佝偻病、粘多糖病Ⅳ型以及干骺发育障碍鉴别的要点),并有散在点状致密影,手足短管骨亦粗短。
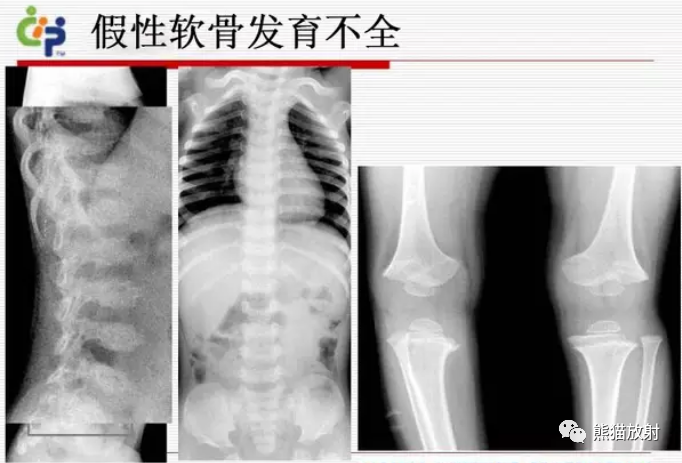
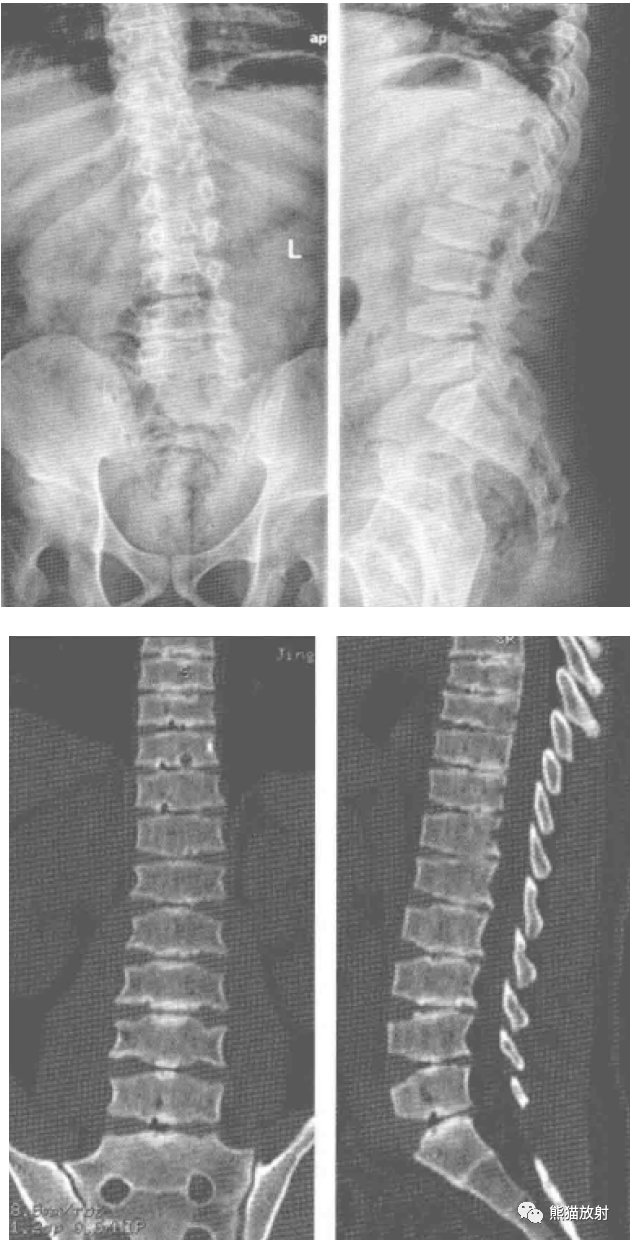
②腰椎椎体后缘轻度凹陷,前部稍呈楔形,正位片上椎弓根间距自上而下逐渐变小(与正常相反)以及坐骨大切迹“鱼口”状改变,为本病特征性表现。
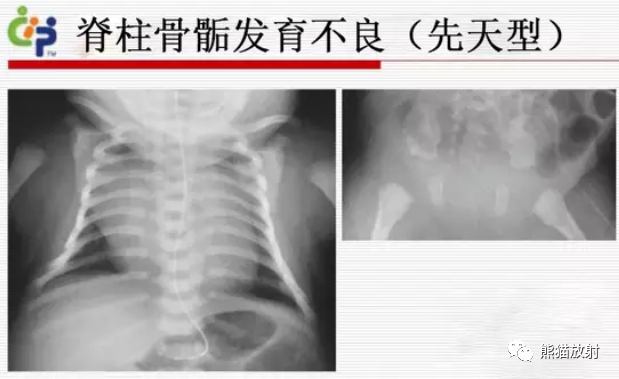
脊柱骨骺发育不良分为哪四型?诊断要点是什么?
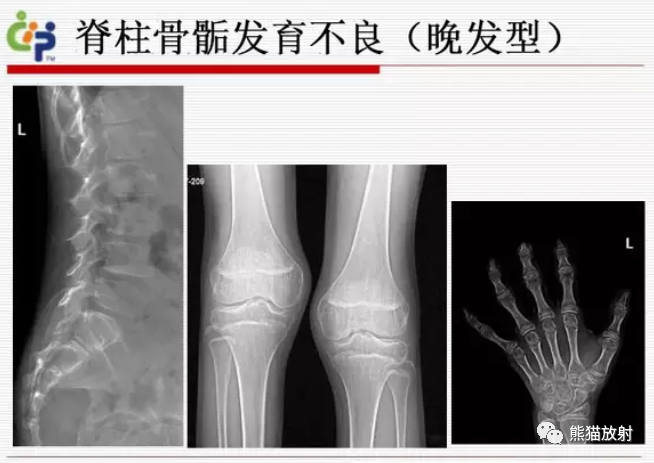
晚发型
迟发型脊柱骨骺发育不良伴进行性关节病
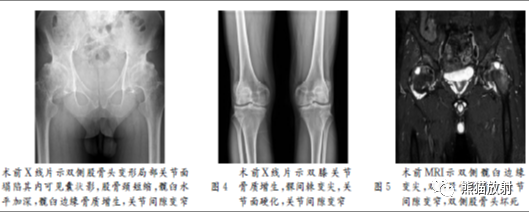
多发性骨骺发育不良的诊断要点是什么?



干骺发育不良有何X线特点?分为几型?
(1)景森 (Jansen) 型:很少见,无家族遗传性,出生时即见异常。病变主要累及长管状骨的干骺端,分布对称,尤以下肢髋、膝、踝部最明显。
(2)施密特(shmid)型:系常染色体显性遗传,多于3~4岁以后出现异常。股骨近端颇具特征:股骨颈粗短,结构不规则,骺板呈垂直位且增宽,髋内翻,头正常。下肢长管状骨可变短和弯曲。
(3)施巴尔(spahr)型:为常染色体隐性遗传,干骺端轻度不规则,但下肢骨常有明显的弯曲畸形。
Schmid型干骺端软骨发育异常

女,5岁,身材矮小,头面部发育正常,神清合作,智力正常,轻度髋内翻鸭步态,躯干短小,双膝内翻畸形。图1:双手2~4指骨短而粗(白箭头),双手掌骨干骺端加宽外展呈杯口状陷凹,临时钙化带不整,部分消失,部分致密,厚薄不均。骺骸嵌入陷凹中,并变形和变大(黑长箭示)。腕骨二次骨化中心有3块。尺骨骺板斜陷,临时期钙化带厚薄不均,但以增厚硬化为主。桡骨中心部反致密增厚、骺核陷入其中,内见不规则的钙化斑(黑箭示) 图2:双髋臼缘变浅拉长,边缘不整,临时钙化带明显厚薄密度不均,其内亦可见大小不等不规则钙斑,以髂骨侧为重。股骨颈变短增宽,颈干角:右为145°,左为148°,股骨干骺稍加宽内凹,临时钙化带略不整。大粗隆骺大而不规则。股骨干颈宽而短(图2)。
半肢骨骺发育异常的诊断要点是什么?

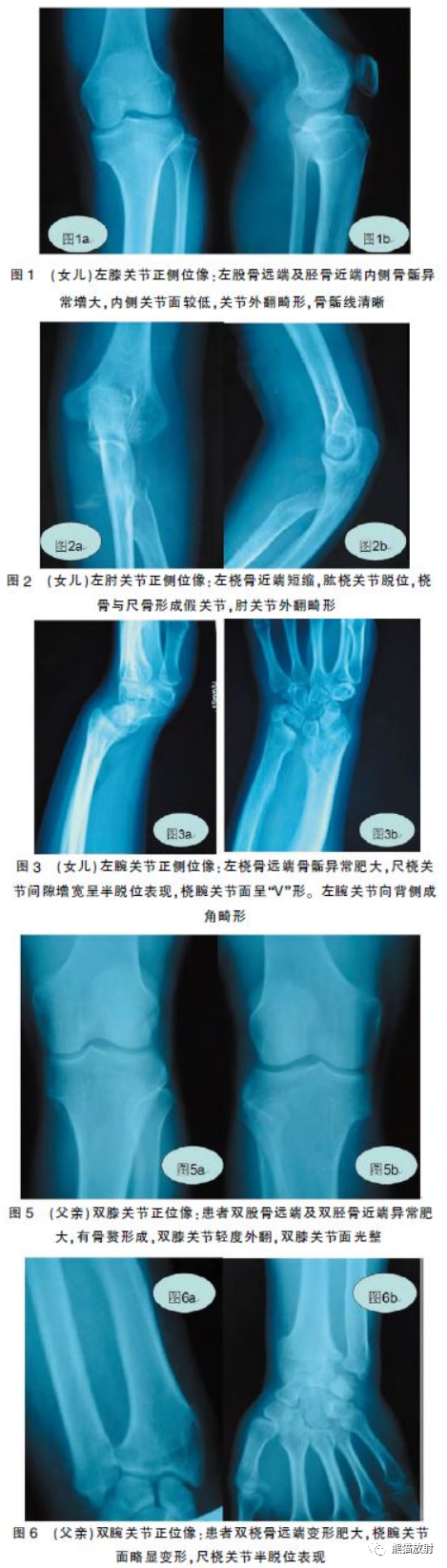
患者,女,14岁。查体:神志清,营养及发育正常,心肺正常。左膝关节、左肘关节及双腕关节畸形,关节周围可触及硬性包块,其中左膝关节内侧肿块约2.5 cm×3.1cm,关节呈外翻畸形。双前臂向背侧弯曲,略短缩。双腕关节背侧可触及大小约2.3 cm×2.5cm大小的肿块,皮肤未见明显异常改变。
患者,男,38岁。查体:正常面容,双膝呈外翻畸形,关节内侧均可触及硬性包块,大小约2.4 cm×3.0cm;双腕关节外侧呈对称硬性包块,轻度畸形改变,双肘关节未见明显异常。
女儿:左股骨远端及左胫骨近端内侧骨骺增大,关节面清晰,内侧关节面略低;左桡骨近端短缩,近端尺桡关节脱位;左腕关节畸形,尺桡骨远端骨骺增大,桡腕关节面呈“V”形,尺桡骨向背侧弯曲(图1~3);父亲:双股骨远端内侧及双胫骨近端内侧关节面下异常肥大,关节间隙未见明显异常;双桡骨远端外侧肥大,尺桡关节间隙略增宽。双腕关节畸形,桡骨干略向背侧侧成角畸形,以上软组织未见明显异常(图5ab,6ab)。
以上文字内容节选自《放射诊断要点与难点解析》(田军、孟庆学主编)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#发育异常#
43
#X线#
45
#发育#
32
#发育不良#
0
#诊断要点#
45
系统,使用标准12导联心电图信息非侵
58
积分
62