HUMAN BRAIN MAPPING:你的痛点有多高,岛叶皮质来决定
2021-07-24 MedSci原创 MedSci原创
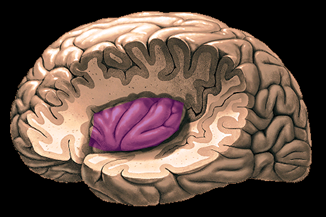
后部IC不仅对于一般的疼痛感知,而且对于确定个体疼痛阈值也是如此。
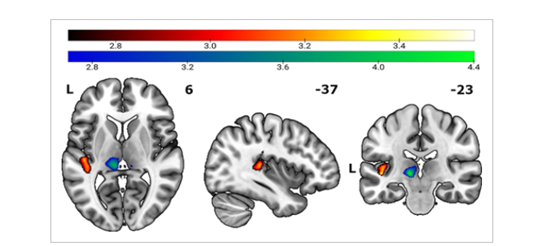
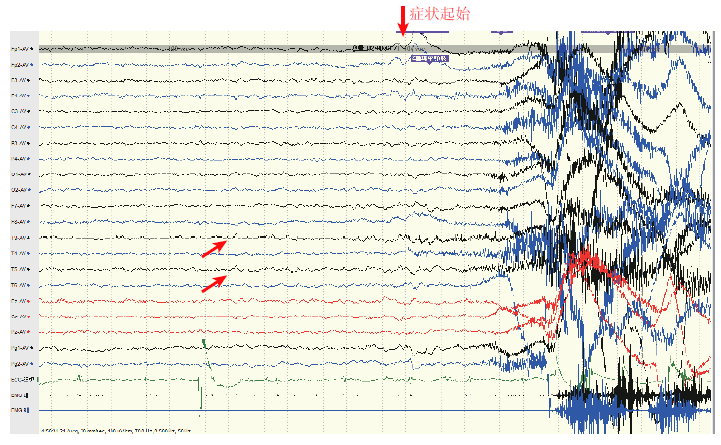
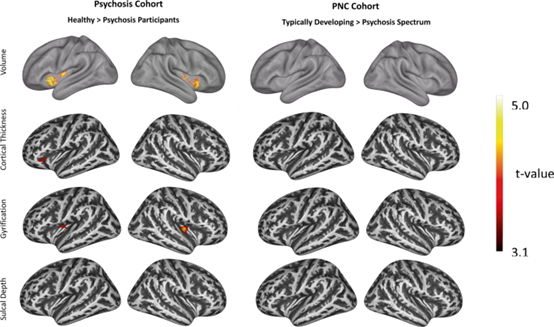
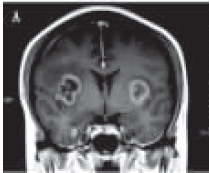
疼痛被定义为与实际或潜在的组织损伤相关或类似于相关的不愉快的感觉和情感体验,其中疼痛阈值标志着对刺激的感知强度增加曲线上的点,在该点开始感觉到疼痛。痛阈在不同个体之间有很大差异,它们在不同时间内经历了个体间的波动。许多行为/心理特征、遗传因素和神经生物学因素已被确定影响疼痛感知的各个方面,例如痛阈、疼痛耐受和疼痛调节。然而,解释这些差异的神经生物学基础仍有待充分阐明。 在HUMAN BRAIN MAPPING杂志最近刊发的研究文章中,Tobias Schmidt-Wilcke等使用基于体素的形态计量学(VBM)和图论,特别是基于静息态功能连接的局部聚类系数(CC),来识别大脑区域,其中区域灰质体积和网络特性预测个体痛阈。 在研究疼痛敏感性的神经相关性时,没有研究将脑形态与脑功能联系起来,特别是RS-FC和网络参数。在此背景下,该研究还进行了VBM分析,寻找区域灰质(GM)体积与疼痛敏感性相关的大脑区域。探讨了在某些脑区,网络参数(例如局部CC)和形态参数(即区域GM体积)是否会一致,表明这两种测量方法虽然来自不同的脑成像方法,但不仅与人类感知有关,而且相互关联,表明大脑功能和结构之间存
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#human#
36
#mapping#
35
非常受用
55
非常受用
55
非常受用
64
学到了#学习#
46