AJRCCM:肺动脉高压血流动力学及右心衰竭
2021-10-15 刘少飞 MedSci原创
事实上,当今 PAH 的主要目标是早期诊断以迅速开始治疗以实现最小的症状负担;优化患者的生化、血流动力学和功能特征;并限制不良事件。为此,临床医生必须熟悉新的危险因素和修订后的 PAH 血流动力学定义

事实上,当今 PAH 的主要目标是早期诊断以迅速开始治疗以实现最小的症状负担;优化患者的生化、血流动力学和功能特征;并限制不良事件。为此,临床医生必须熟悉新的危险因素和修订后的 PAH 血流动力学定义。
进一步完善的 PH 血流动力学
mPAP ⩾ 25 mm Hg 的经典 PH 定义主要基于专家共识意见,没有规范或结果数据。 2009 年,Kovacs 及其同事确定正常 mPAP 的上限为 20 毫米汞柱,显示的年龄差异很小。这些数据与来自大型 RHC 转诊人群的发现一致,其中全因死亡风险从 19-20 毫米汞柱开始并持续上升到 40 毫米汞柱。在表型良好的 SSc 患者和混合性心肺疾病患者中,mPAP < 25 mmHg 也与运动能力受损和不良临床事件独立相关。根据这些集体数据,强烈建议将 PH 的诊断标准从 ⩾ 25 毫米汞柱更改为 > 20 毫米汞柱。
尽管降低 mPAP 阈值可以捕获更多高危患者,但某些生理状况(例如,怀孕)和可立即逆转的高肺流量状态(例如,贫血)可以升高 mPAP,而没有 PVR 升高的证据。这一点很重要,因为升高的肺动脉压 (PAP) 本身并不是肺血管疾病的特征。正如 Wood 在 1958 年最初描述的那样(“多动”或高流量状态可能会提高 PAP。在流量增加的条件下,预计 PVR 会降低。因此,为了优化 mPAP 诊断的特异性肺血管疾病本身,PVR ⩾ 3.0 WU被添加到描述毛细血管前表型的标准中。这可能是一个保守的阈值,有利于肺血管疾病的晚期诊断;然而,在门肺动脉高压或镰状细胞瘤患者中观察到危害信号细胞疾病和 PVR < 3.0 WU. 最近的研究表明,与 <2.0 WU相比,SSc-PAH 和 PVR >2.0 WU 的患者死亡率增加,而在 mPAP 升高的大型转诊人群中,死亡率增加从大约 2.2 WU 开始,风险持续增加。此外,轻度升高的 mPAP (20-24 mmHg) 似乎在先前存在左心或肺疾病的患者中更为常见,因此该血流动力学亚组对捕获 PAH 患者的重要性仍不确定。随着我们对长期结果的理解不断加深,当今使用的血流动力学定义可能会进一步完善。
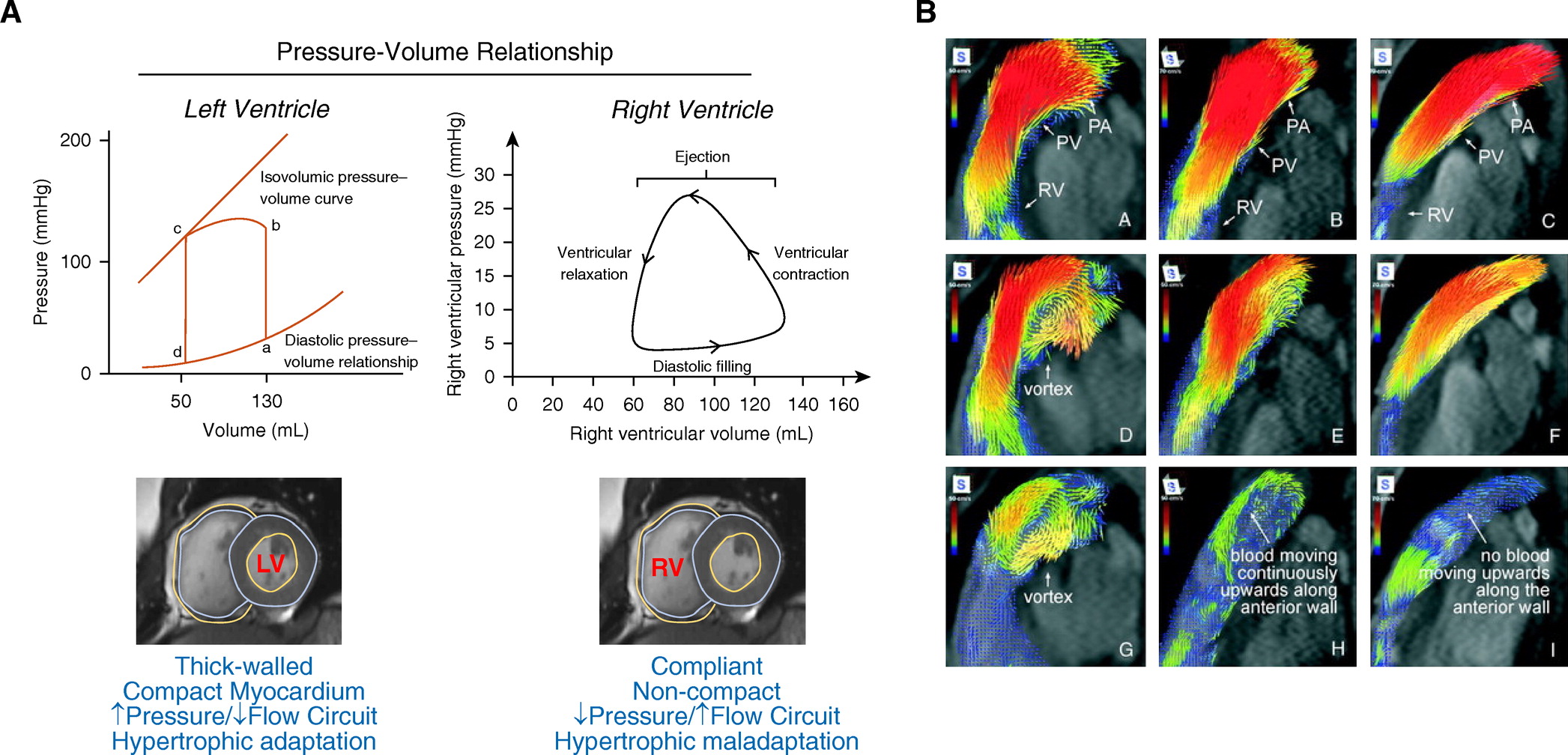
右心与肺动脉高压
肺动脉顺应性(计算为每搏输出量/肺动脉脉压)随着 RV 后负荷的增加而降低,然后 PVR 明显升高。 RV 后负荷的慢性升高迫使有利于强容量脉冲的状态变为具有强压力脉冲的状态。从功能上讲,这与 RV 能量使用平衡向维持肺动脉压的转变有关,以牺牲通常用于肺泡灌注的能量为代价,这被称为“RV-肺动脉 (PA) 解偶联”。总体而言,RV-PA 解偶联是 PAH 进展为心力衰竭和不良结果的前哨病理生理事件。 RV 扩张的倾向和肺血管重塑的程度可能会影响个体患者的 RV-PA(非)偶联曲线(图A)。量化 RV-PA 耦合需要常规实践中无法使用的精密设备;然而,RV-PA 耦合的替代指标,例如三尖瓣环平面收缩压偏移 (TAPSE) 与使用超声心动图或三维磁共振成像测量的估计肺动脉收缩压 (PASP) 的比值,正在成为提供信息和作为为未来的研究建立一个框架,阐明该测量在临床实践中的预后效用(图 B)。
认识 PAH 的全身症状
LV 充盈受损、心律失常、肾功能障碍、神经体液过度激活、骨骼肌功能障碍和充血性肝病是继发于 PH 右心衰竭的终末器官损伤模式。右侧心肾综合征的概念得到了数据的支持,该数据表明在 PAH 血浆中,醛固酮与正常水平相比增加了 2.8 倍,并且在没有左心疾病的情况下与心输出量呈负相关。肾灌注受损对 PAH 的预后很重要;在一项涉及 500 名患者的研究中,血清肌酐 >1.4 mg/dl 与死亡风险风险相关,该风险比水平 <1.0 mg/dl 的患者高 2.4 倍。在评估早期和长期 PAH 疾病管理注册 (REVEAL) 注册中,估计肾小球滤过率从基线下降 10% 且持续 1 年以上的 PAH 患者的肾小球滤过率增加了 66%。他们的死亡风险。右心房压力是 PH 中估计的肾小球滤过率的独立预测因子,表明中枢压力升高引起的肾间质水肿增加可能与 PH 介导的心肾功能障碍有关。还提出由严重升高的 RV 空腔压力和心包约束驱动的正常室间隔动力学的破坏会破坏左心充盈,从而损害心输出量。孤立性右心衰竭患者嗜盐所特有的潜在病理生理学可能涉及肾素-血管紧张素-醛固酮轴的过度激活,但需要进一步研究来阐明这一点。
代谢功能障碍,包括胰岛素抵抗和脂肪酸代谢受损,在 PAH 中很常见,并导致血液动力学紊乱。营养不良、肥胖、恶病质和肌肉减少症也被证实或可能与 PAH 相关,并且与(极端)营养对疾病发病机制的贡献一致。例如,抗坏血酸(维生素 C)是氧化酶(包括内皮糖蛋白)催化的各种反应的还原剂和辅助因子。内皮糖蛋白羟基化 HIF-1α 以促进其降解;反过来,受损的 HIF-1α 降解与增加的 HIF-1α 依赖性肺血管收缩和 PAH 中的不利血管重塑有关。这可以解释将坏血病与偶发性(尽管是可逆的)PAH系起来的证据汇合线。
参考文献:
Maron BA, Abman SH, Elliott CG, Frantz RP, Hopper RK, Horn EM, Nicolls MR, Shlobin OA, Shah SJ, Kovacs G, Olschewski H, Rosenzweig EB. Pulmonary Arterial Hypertension: Diagnosis, Treatment, and Novel Advances. Am J Respir Crit Care Med. 2021 Jun 15;203(12):1472-1487. doi: 10.1164/rccm.202012-4317SO. PMID: 33861689; PMCID: PMC8483220.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#血流动力#
40
#心衰竭#
55
#右心衰竭#
44
#RCC#
41
#动脉高压#
23
#右心衰#
44
#血流动力学#
37