我国急性冠心病年轻化趋势明显
2015-01-26 刘军, 赵冬, 刘静等.2006至2012年急性冠状动脉综合 中国循环杂志
我国急性冠心病年轻化趋势明显:6年两次调查发病年龄下降3岁 我们经常说,中国的冠心病年轻化趋势明显,但怎么体现呢?北京安贞医院刘军和赵冬等的一项发现,2006年中国急性冠脉综合征患者平均年龄是64.7岁,而2012年平均年龄则降低至61.9岁,平均降低了3岁左右。 2006年中青年(≤60岁)的比例占32.1%,2012年则占到了42.5%。增加了32.4%。男性的年轻化
我国急性冠心病年轻化趋势明显:6年两次调查发病年龄下降3岁
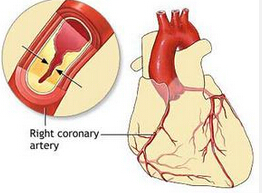
我们经常说,中国的冠心病年轻化趋势明显,但怎么体现呢?北京安贞医院刘军和赵冬等的一项发现,2006年中国急性冠脉综合征患者平均年龄是64.7岁,而2012年平均年龄则降低至61.9岁,平均降低了3岁左右。
2006年中青年(≤60岁)的比例占32.1%,2012年则占到了42.5%。增加了32.4%。男性的年轻化更明显,2012年男性患者年龄<55岁为36.1%,比2006年的28.7%增加了25.8%。
研究还发现,2012年ACS 患者伴有高血压、高胆固醇血症、糖尿病的比例较2006年均显著增加,尤其是伴有高胆固醇血症的患者,较6年前增加了2.1倍。
当然,急性冠状动脉综合征的临床诊治水平也在提高。比如,使用经皮冠脉介入治疗(PCI)和循证医学证实有效的二级预防药物的使用率也有所提高,尤其是氯吡格雷和他汀类药物的使用。
2012年β受体阻滞剂和血管紧张素转换酶抑制剂或血管紧张素Ⅱ受体拮抗剂的使用率却较2006年有所下降。
研究者分别于2006年在全国31个省、自治区和直辖市65家医院(中国冠心病二级预防架桥工程I期研究)和2012 年在全国21个省、自治区和直辖市34家医院(中国冠心病二级预防架桥工程Ⅲ期研究)连续入选≥18岁的住院冠心病患者332例和3391例。排除因外伤入院并怀疑ACS者及已参加任何一项药物临床试验者。将其中调查资料完整的ACS患者纳入本研究,2次调查的有效病例数均为3124例。
来源:刘军, 赵冬, 刘静等.2006至2012年急性冠状动脉综合征住院患者诊疗状况的变化.中华心血管病杂志2014,42:957.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









已阅
90
明白
127
#急性冠心病#
0
这个结果不可靠
122
too young !
154
too young to single
107
too young to single
83