J Gastroenterol Hepatol:MRE在预测慢性肝病患者腹水存在方面具有较高的诊断效能
2018-04-12 MedSci MedSci原创
与血清纤维化标志物相比,MRE在预测腹水存在方面具有较高的诊断效能。基于肝硬度测量的LSMRE具有预测CLD患者腹水存在的潜力。
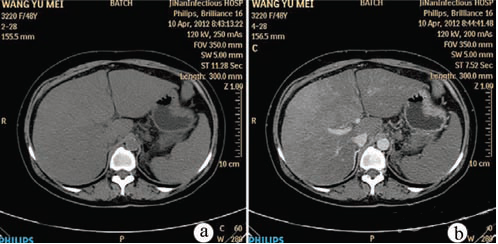
研究目的:本研究旨在评估磁共振弹性成像(MRE)是否能作为一种非侵入性方法预测慢性肝病(CLD)患者是否会发生腹水。
研究方法:从2013年3月至2015年6月,208例CLD患者进行了肝硬度测量。采用受试者工作特征(ROC)曲线评价MRE预测患者发生腹水的诊断效能,并与其他血清纤维化标志物的表现进行比较。进行多因素logistic回归分析,以确定与腹水存在相关的危险因素。在基线时,对无腹水的患者出现腹水的累积发病率进行了检查。81例CLD患者行病理组织学诊断,对肝纤维化病理分期进行评价。
研究结果:在208例患者中,41例患者发生腹水。存在腹水的最佳LS临界值为6.0 kPa (ROC曲线下面积= 0.87)。出现腹水时,MRE的ROC曲线下面积显著高于其他肝纤维化标志物的曲线下面积。多因素分析显示,LS >6.0 kPa是腹水存在的独立危险因素。LS值>6.0 kPa的患者,腹水累积发生率显著增高。在诊断肝纤维化分期≥4的患者时,MRE相比于其他肝纤维化指标的准确性更高。
研究结论:与血清纤维化标志物相比,MRE在预测腹水存在方面具有较高的诊断效能。基于肝硬度测量的LSMRE具有预测CLD患者腹水存在的潜力。
原始出处:
Abe K, Takahashi A, Imaizumi H, et al. Utility of magnetic resonance elastography for predicting ascites in patients with chronic liver disease. J Gastroenterol Hepatol, 2018, 33(3), 733-740. doi: 10.1111/jgh.13927.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#GAS#
38
#Gastroenterol#
44
#肝病患者#
43
#MRE#
42
#AST#
31
#EPA#
36