PLoS One:血肌酐可预测血透患者死亡风险
2016-05-31 phylis 译 MedSci原创
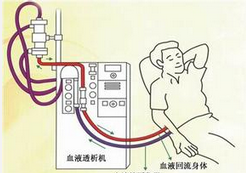
背景:高体重指数(BMI)与血液透析(HD)患者疗效较好相关。本研究旨在探讨血清肌酐(Cr)这种肌肉质量的标记物,是否可以改变HD患者BMI与死亡率和发病率的关系。方法:日本的研究者从日本透析治疗登记的全国性的数据库中获得数据,进行回顾性的研究。共入选患者119099例(年龄:65±12岁,HD的中位数时间为5.6年,男性占62%),研究者探讨了1年后BMI与死亡率和发病率的相关性。按照BMI将患
背景:高体重指数(BMI)与血液透析(HD)患者疗效较好相关。本研究旨在探讨血清肌酐(Cr)这种肌肉质量的标记物,是否可以改变HD患者BMI与死亡率和发病率的关系。
方法:日本的研究者从日本透析治疗登记的全国性的数据库中获得数据,进行回顾性的研究。共入选患者119099例(年龄:65±12岁,HD的中位数时间为5.6年,男性占62%),研究者探讨了1年后BMI与死亡率和发病率的相关性。按照BMI将患者分为4组,或者按照血肌酐水平分成3组。应用多元回归分析法计算OR值和95%CI。
结果:高BMI不能预测1年总死亡率。然而,按照血肌酐将患者分层时,最低血肌酐水平的肥胖患者,心脏死亡的风险显著升高,男性OR值为2.82 [ 1.51-5.27 ],女性的OR值为2 [ 1.03-3.90 ]。最低的血肌酐水平肥胖男性患者,心脑梗死的风险较高。相反,高水平血肌酐的非肥胖患者,心脏、脑血管和感染相关的死亡水平显著降低。高血肌酐与非肥胖HD患者心血管事件风险降低相关。
结论:血液透析患者出现的肥胖的悖论,仅适用于用体重指数定义肥胖时。血肌酐水平较低与所有BMI患者不良预后相关。因此,无论患者体重指数如何,一旦接受常规血液透析,血肌酐水平均可用于预测死亡的发生。
原始出处:
Sakao Y, Ojima T, et al. Serum Creatinine Modifies Associations between Body Mass Index and Mortality and Morbidity in Prevalent Hemodialysis Patients. PLoS One. 2016 Mar 1.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Plos one#
29
#患者死亡#
33
#死亡风险#
36
#肌酐#
35
#血肌酐#
43
#血透#
32